Tacrolimus Neurotoxicity: Signs, Risks, and What You Need to Know
When you take tacrolimus, a powerful immunosuppressant used after organ transplants to prevent rejection. Also known as FK506, it keeps your body from attacking the new organ—but it doesn’t always play nice with your brain. Even at the right dose, tacrolimus can cause serious neurological side effects. This isn’t rare. Studies show up to 20% of transplant patients on tacrolimus report some form of neurotoxicity, and for some, it’s severe enough to require a drug change.
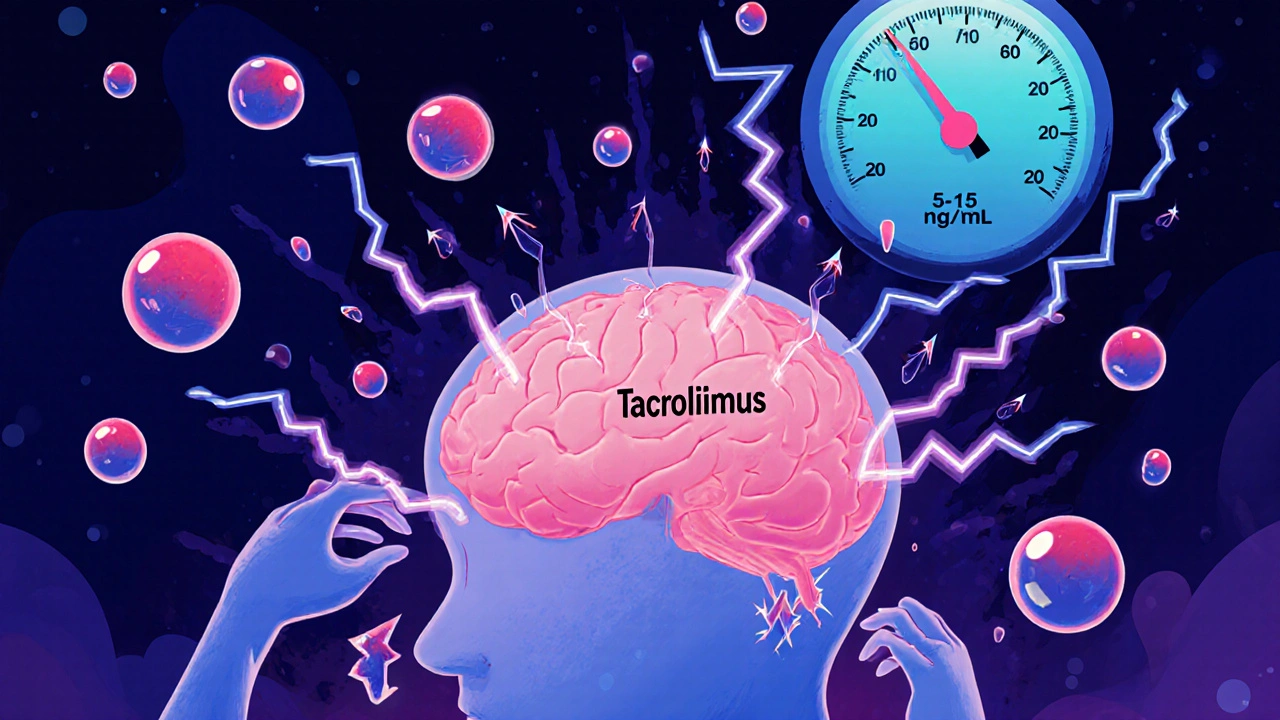
The brain doesn’t have a safety switch for this drug. tacrolimus neurotoxicity, a direct toxic reaction to the drug in the central nervous system shows up in ways you might not expect: headaches that won’t quit, shaky hands, trouble speaking clearly, or sudden confusion. In worse cases, patients experience seizures, vision changes, or even coma. These aren’t side effects you can ignore—they’re red flags that need immediate attention. What makes it tricky is that these symptoms often look like other problems: a migraine, stress, or even a stroke. That’s why doctors monitor blood levels closely, especially in the first few weeks after transplant.
Some people are more at risk than others. If you’re older, have kidney problems, or are taking other drugs that affect how tacrolimus is broken down—like certain antifungals or antibiotics—you’re more likely to run into trouble. Even small changes in your dose or diet can push levels into dangerous territory. It’s not just about the number on the bottle; it’s about how your body handles it. That’s why regular blood tests aren’t optional—they’re lifesavers.
And it’s not just the drug itself. immunosuppressant neurotoxicity, a broader category that includes reactions to drugs like cyclosporine and sirolimus shares common patterns with tacrolimus. The brain is sensitive to these compounds because they cross the blood-brain barrier easily. That’s why switching from one immunosuppressant to another doesn’t always fix the problem—it just changes the shape of the risk.
You won’t find this in every patient, but when it hits, it hits hard. That’s why knowing the early signs matters. If you’re on tacrolimus and start feeling off—not just tired, but mentally foggy, dizzy, or twitchy—don’t wait. Tell your doctor. Catch it early, and you might avoid hospitalization. Adjust the dose, swap the drug, or treat the symptoms before they spiral.
Below, you’ll find real-world cases and practical advice from patients and doctors who’ve dealt with this. You’ll learn how to spot trouble before it escalates, what blood levels to watch for, and which other medications can make things worse. This isn’t theoretical—it’s the kind of info that keeps people out of the ER and helps them stay healthy after transplant.