Tacrolimus Blood Levels: What You Need to Know About Monitoring and Safety
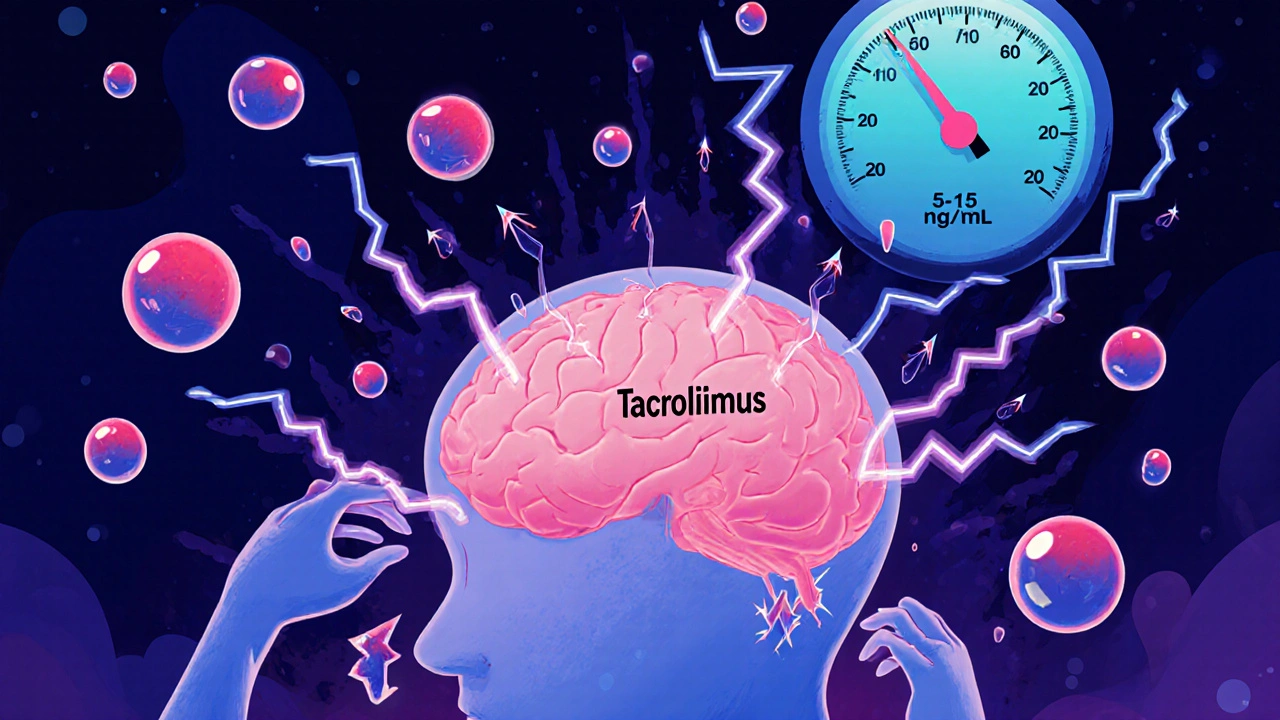
When you're taking tacrolimus, an immunosuppressant drug used mainly after organ transplants to prevent rejection. Also known as FK506, it works by calming your immune system—but only if your blood levels stay in the right range. Too low, and your body might attack the new organ. Too high, and you risk kidney damage, nerve problems, or even life-threatening toxicity. That’s why tracking tacrolimus blood levels isn’t optional—it’s the difference between a successful transplant and a medical emergency.
Tacrolimus doesn’t work the same for everyone. Your levels depend on your weight, liver function, what else you’re taking, and even what you ate that day. Certain foods like grapefruit can spike your levels. Antibiotics, antifungals, and even St. John’s wort can mess with how your body processes it. That’s why doctors don’t just give you a pill and walk away—they order regular blood tests, often weekly at first, then every few weeks. The goal? Keep your levels between 5 and 15 ng/mL for most adult transplant patients, though exact targets vary by organ and time since surgery.
It’s not just about the number. Symptoms matter too. If you start having tremors, headaches, blurry vision, or unusual swelling, your levels might be too high. If you feel more tired than usual, develop a fever, or notice reduced urine output, your levels could be too low. These signs often show up before blood tests do. That’s why patients on tacrolimus need to be their own advocates—track your symptoms, know your last level, and speak up when something feels off.
Related to this, drug interactions, how one medication changes how another works in your body. Also known as pharmacokinetic interference, it’s a major reason why tacrolimus levels swing unpredictably. For example, if you’re prescribed an antifungal like ketoconazole for a yeast infection, your tacrolimus level could jump overnight. Same goes for some blood pressure meds, seizure drugs, or even over-the-counter antacids. That’s why every new prescription—even something simple like ibuprofen—needs to be checked against your transplant meds.
And let’s not forget timing. Tacrolimus is usually taken twice a day, 12 hours apart. But if you take it with food, especially fatty meals, absorption drops. That’s why most guidelines say to take it on an empty stomach—either one hour before or two hours after eating. Skip a dose? Don’t double up. Call your clinic. Missed doses or late blood draws can throw off your whole treatment plan.
What you’ll find in the posts below are real-world stories and clear guides on how other patients manage similar meds—like how coffee affects levothyroxine, how calcium interferes with bisphosphonates, or why splitting pills can be dangerous. These aren’t abstract theories. They’re lessons from people who’ve been there. If you’re on tacrolimus, you’re not just following a prescription—you’re managing a delicate balance. The information here will help you do it smarter, safer, and with fewer surprises.