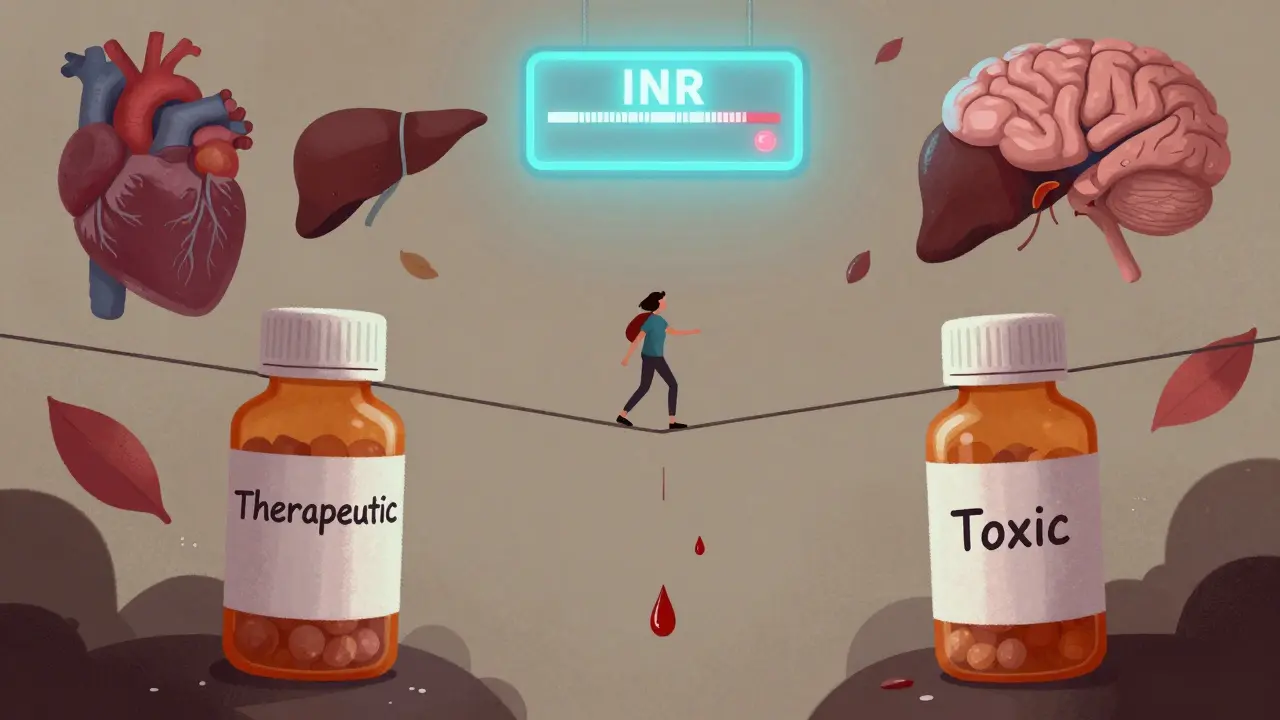
Some medications are like walking a tightrope. Take one step too far, and you could fall into serious danger - too little, and the treatment doesn’t work. These are NTI drugs, or Narrow Therapeutic Index drugs. They have almost no room for error. A tiny change in dose - even 10% - can mean the difference between healing and hospitalization. If you or someone you know takes one of these, understanding what they are and how they work isn’t just helpful - it’s life-saving.
What Makes a Drug an NTI Drug?
An NTI drug has a very small gap between the dose that works and the dose that harms. Think of it like a thermostat set to 72°F. If it jumps to 75°F, your house gets too hot. If it drops to 69°F, you’re shivering. With NTI drugs, the margin is even tighter - sometimes just a few nanograms per milliliter in your blood.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in blood levels can cause serious side effects or treatment failure. That’s why these drugs aren’t treated like regular pills. Even switching from one brand to a generic version can cause problems if the body absorbs it slightly differently. That’s why pharmacists and doctors monitor these drugs closely - often with regular blood tests.
Top NTI Drugs You Need to Know
There are dozens of NTI drugs, but these are the most common ones you’ll see in clinics, hospitals, and prescriptions:
- Warfarin - An anticoagulant used to prevent blood clots. The target is an INR of 2.0-3.0. Go above 4.0, and bleeding risk spikes by over 7 times. A 10% dose increase can push someone into danger.
- Lithium - Used for bipolar disorder. The therapeutic range is 0.6-1.2 mmol/L. At 1.5 mmol/L, you risk tremors, confusion, and kidney damage. Many patients miss their blood tests - and that’s when things go wrong.
- Digoxin - For heart failure and irregular heartbeat. The safe window is 0.5-2.0 ng/mL. Levels above 2.0 can cause nausea, vision changes, and deadly heart rhythms.
- Phenytoin - An anti-seizure drug. Therapeutic range: 10-20 mcg/mL. Too high? You get dizziness, slurred speech, and even coma. Too low? Seizures return.
- Tacrolimus - A transplant drug. Levels must stay between 5-15 ng/mL. Even a 2 ng/mL drop can trigger organ rejection. Transplant patients get blood drawn 3 times a week at first.
- Levothyroxine - For hypothyroidism. Small changes in dose can swing TSH from normal (1.2) to dangerously high (8.7), causing fatigue, weight gain, and heart issues. One Reddit user reported a patient’s TSH jumped after switching generic brands - it took three months to stabilize.
- Carbamazepine - Another seizure and nerve pain drug. Therapeutic range: 4-12 mcg/mL. Too high? Liver damage. Too low? Seizures.
- Cyclosporine - Used in organ transplants and autoimmune diseases. Range: 100-400 ng/mL. A 10% drop can lead to rejection. Many transplant centers don’t allow generic switches without doctor approval.
- Valproic acid - For epilepsy and mood disorders. Safe range: 50-100 mcg/mL. Levels above 150 can cause liver failure.
These aren’t just numbers on a chart. These are real thresholds that determine whether someone stays healthy or ends up in the ER.
Why Generic Substitutions Can Be Risky
For most drugs, switching from brand to generic is safe and saves money. Not with NTI drugs.
The FDA requires stricter bioequivalence testing for these. While regular generics must be within 80-125% of the brand’s absorption, NTI generics must stay within 90-111%. That’s a tighter net. But even then, small differences in how the body absorbs the drug can add up over time.
States have different rules. North Carolina, Oklahoma, and 28 other states require doctors to specifically write “dispense as written” on prescriptions for NTI drugs. That means pharmacies can’t swap generics without permission. In some places, pharmacists still try to substitute - and patients end up with unstable levels.
One study found that 73% of hospital pharmacists have personally stopped a dangerous NTI substitution in the past year. That’s not a rare event - it’s standard practice.
Monitoring Isn’t Optional - It’s Essential
You can’t guess your way through an NTI drug. Blood tests aren’t suggestions - they’re requirements.
- Warfarin: INR checked weekly at first, then every 2-4 weeks once stable.
- Lithium: Every 3-6 months, but more often if you’re sick, dehydrated, or starting a new medication.
- Tacrolimus: 3x weekly after transplant, then weekly, then monthly - depending on stability.
- Phenytoin: Trough levels checked every 1-2 weeks after a dose change.
These tests cost $25-$150 each. Medicare covers 80%, but copays add up. And 32% of lithium patients miss appointments - often because they feel fine. That’s the danger: you don’t feel the toxicity until it’s too late.
Only 45% of hospital systems have automated alerts when NTI levels go out of range. That means many errors are caught by alert pharmacists - not computers.
Emerging NTI Drugs: The New Frontier
The list isn’t static. New drugs, especially in cancer care, are joining the NTI group.
Targeted therapies like axitinib (for kidney cancer), ponatinib (for leukemia), and olaparib (for ovarian cancer) now have defined therapeutic ranges. Axitinib’s target is 15-30 ng/mL. Too low? The tumor grows. Too high? Severe high blood pressure, liver damage, or heart failure.
Even newer anticoagulants like apixaban and rivaroxaban are under review by the FDA for NTI status. While they’re often called “safer” than warfarin, experts warn their narrow window still demands caution - especially in older adults or those with kidney issues.
By 2023, 23% of newly approved cancer drugs had narrow therapeutic indices - more than double the rate of all new drugs. Precision medicine means more precision dosing - and more risk if it’s off.
What You Can Do to Stay Safe
If you’re on an NTI drug, here’s what matters most:
- Never switch brands or generics without talking to your doctor. Even if the pharmacy says it’s “the same,” it might not be.
- Keep all blood test appointments. Even if you feel fine. Symptoms often appear too late.
- Track your doses and side effects. Write down when you feel dizzy, nauseous, or unusually tired. Bring it to your next visit.
- Ask about drug interactions. Antibiotics, grapefruit juice, and even over-the-counter painkillers can throw off NTI levels.
- Know your target range. Don’t just take the pill - know what your blood level should be.
There’s no room for guesswork. These drugs work - but only when they’re precisely managed.
The Bigger Picture
NTI drugs make up only about 15% of medications that require blood monitoring - but they cause 30% of dosing-related hospitalizations. That’s not a coincidence. It’s a system failure waiting to happen.
As more cancer drugs, biologics, and psychiatric medications enter this category, the pressure on healthcare systems grows. AI tools are being tested to predict dosing errors before they happen. One pilot study cut NTI-related adverse events by 28% using smart alerts.
But technology alone won’t fix this. It takes awareness. It takes communication between patients, doctors, and pharmacists. It takes the courage to say: “I need to stick with this brand.” “I need that blood test.” “I’m not feeling right - let’s check my levels.”
NTI drugs aren’t dangerous because they’re bad. They’re dangerous because they’re powerful. And power, when handled carefully, saves lives. When handled carelessly, it ends them.
Are all blood thinners NTI drugs?
No. Warfarin is an NTI drug because its therapeutic window is extremely narrow and affected by diet, other medications, and genetics. Newer blood thinners like apixaban, rivaroxaban, and dabigatran have wider therapeutic ranges and don’t require routine blood monitoring. However, the FDA is reviewing whether some of these should be classified as NTI due to bleeding risks in certain populations.
Can I switch from brand to generic NTI drugs if it’s cheaper?
It’s not recommended without your doctor’s approval. Even FDA-approved generic NTI drugs can have slight differences in absorption. One patient’s TSH jumped from 1.2 to 8.7 after switching generic levothyroxine brands - it took three months to stabilize. Always ask your doctor if switching is safe for your specific drug.
Why do some states restrict generic substitution for NTI drugs?
Because small differences in drug absorption can lead to treatment failure or toxicity. States like North Carolina and Oklahoma have laws requiring doctors to explicitly approve any substitution. This isn’t about profit - it’s about preventing avoidable hospitalizations and deaths.
Do I need to get blood tests forever if I’m on an NTI drug?
Not forever - but regularly. Once your levels are stable for 6-12 months, tests may drop from weekly to monthly or quarterly. But if you get sick, start a new medication, change your diet, or gain/lose weight, your levels can shift. Always check with your provider before reducing monitoring.
What should I do if I miss a dose of an NTI drug?
Don’t double up. Call your doctor or pharmacist immediately. For drugs like warfarin or lithium, skipping a dose can cause clotting or seizure risk. For others, it might cause withdrawal or rebound symptoms. The right action depends on the specific drug - so don’t guess. Get professional advice.
Final Thought: Precision Is the Point
NTI drugs aren’t meant to be taken lightly. They’re tools of precision - used when the stakes are high and the margin for error is razor-thin. They work wonders for heart failure, seizures, transplants, and mood disorders - but only when managed with care.
If you’re on one, you’re not just a patient. You’re part of a team: your doctor, your pharmacist, your lab, and you. Stay informed. Ask questions. Don’t skip tests. And never assume a generic is the same unless your doctor says so.
Because with NTI drugs, the difference between safe and dangerous isn’t just a number. It’s your life.

Comments (14)
Nancy Kou
This is one of those posts that should be mandatory reading for every patient on chronic meds. I work in pharmacy and see the fallout from sloppy NTI management every week. People think 'it's just a pill' until they're in the ER with a TSH of 12 or a digoxin level that could power a small city. Knowledge saves lives here.
Nicole Rutherford
Let’s be real - most doctors don’t even know what NTI means. I had my lithium dose changed by a PA who thought 'it’s just mood stabilizer' and didn’t check my levels for eight months. I ended up in the psych ward because no one bothered to look at the numbers. The system is broken, and patients are the collateral damage.
Hussien SLeiman
Oh here we go again with the fear-mongering about generics. The FDA has stricter standards for NTI generics than for most other drugs. People panic because they don’t understand pharmacokinetics. I’ve switched my levothyroxine brand three times over the past decade - my TSH has been stable at 1.8 every single time. It’s not magic, it’s science. The real issue is lazy clinicians who refuse to update their 1990s thinking. Stop treating patients like fragile porcelain dolls and start trusting the data.
Guillaume VanderEst
I’m a transplant patient on tacrolimus. They used to draw my blood three times a week. Now? Once a month. They say I’m 'stable.' But I feel it - the tremors, the brain fog, the weird metallic taste. I’ve begged them to check my levels. They say, 'You’re fine.' I’m not fine. I’m just good at hiding it until I collapse. Someone needs to audit this. This isn’t healthcare - it’s cost-cutting with a stethoscope.
Alisa Silvia Bila
Thank you for this. I’m on warfarin and didn’t realize how many things affect it - even kale smoothies. I started tracking everything: meds, food, alcohol, even my sleep. My INR went from wild swings to rock solid. Small changes. Big results.
Janelle Moore
Did you know the FDA is in bed with Big Pharma? They allow generics to be 'close enough' so hospitals can save money - but they know it kills people. That’s why they don’t test every batch. They don’t want to admit the truth: this whole system is designed to make you dependent, not healthy. Your blood test? A revenue stream. Your fear? Their profit margin.
Henry Marcus
NTI drugs? More like N.T.I. - 'Never Trust It.' I’ve seen people die from 'generic' substitutions. The government says it’s safe. The lab reports say otherwise. Who do you believe? The algorithm? Or the guy who woke up with his heart trying to escape his chest? I keep my brand-name pills locked in a safe. And I won’t let anyone near my meds. Not even my pharmacist.
Carolyn Benson
There’s a deeper truth here: we treat medicine like it’s a vending machine. Pop a pill, feel better. But NTI drugs expose the illusion. They force us to confront our own fragility - that we are not in control, that biology doesn’t care about our schedules, our budgets, our convenience. We want to believe science is pure. But it’s not. It’s messy, human, and often neglected. And that’s the real tragedy - not the numbers, but the indifference.
William Liu
Just wanted to say - if you’re reading this and you’re on an NTI drug, you’re doing better than you think. Staying on top of your levels, asking questions, tracking symptoms - that’s courage. Keep going. You’re not alone.
Aadil Munshi
Interesting how Western medicine treats NTI drugs like they’re exotic beasts. In India, we’ve been managing phenytoin and cyclosporine for decades with minimal monitoring - because we don’t have the luxury of weekly blood draws. We rely on clinical judgment, patient feedback, and community knowledge. Maybe the problem isn’t the drugs - it’s the over-reliance on labs and under-reliance on human intuition. The algorithm doesn’t know when a patient is lying about their adherence.
Glen Arreglo
I’m a nurse in a rural clinic. We don’t have a lab on-site. We send out blood tests and wait 3-5 days. Patients miss appointments because they can’t take time off work. We’re doing our best - but this system is set up to fail people like mine. I wish we had better tools, not just more rules.
Ashley Bliss
Let me guess - this post was sponsored by the brand-name drug companies. Why else would they scare people away from generics? You know what’s really dangerous? People who think they’re entitled to the most expensive version of everything. Your insurance doesn’t care. Your body doesn’t care. Stop buying into the fear. Trust the science - not the fearmongers.
Dev Sawner
It is imperative to acknowledge that the current regulatory framework governing the bioequivalence of narrow therapeutic index pharmaceuticals is fundamentally inadequate. The 90-111% bioequivalence criterion, while statistically acceptable under current guidelines, does not account for inter-individual pharmacokinetic variability, particularly in elderly populations with polypharmacy. A paradigm shift toward personalized therapeutic drug monitoring is not merely advisable - it is ethically obligatory.
Moses Odumbe
NTI drugs = 🚨⚠️💣 I’ve seen a guy go from fine to coma in 48 hours because his pharmacist swapped his phenytoin. He didn’t even know it happened. Now I bring my own pills to the hospital. I label them. I take pictures. I email my doctor. If you’re not doing this, you’re playing Russian roulette with your brain. 💊🔥