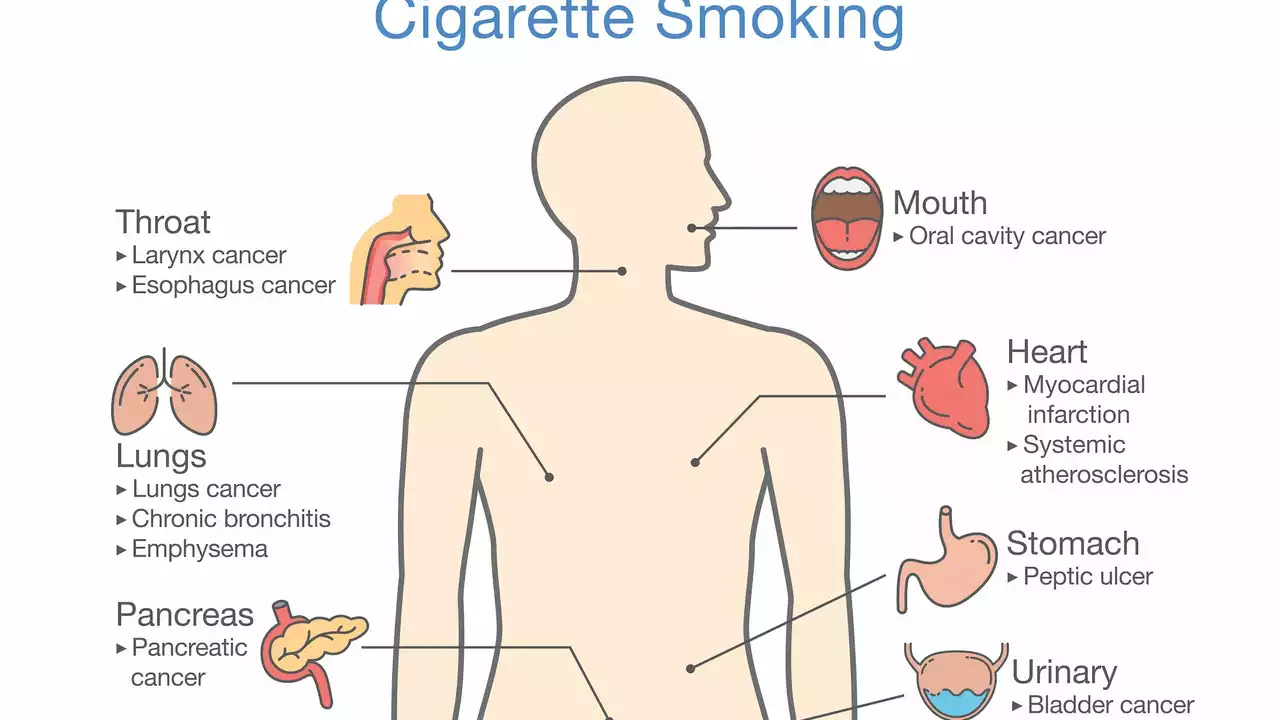
Smoking: practical steps to quit, what changes in your body, and why meds matter
You don’t have to wait years to feel better after you stop smoking. A lot of positive changes start within minutes, and some medications you take now can act differently if you smoke or if you stop. This page gives short, useful steps to quit, a clear timeline of benefits, and the key drug interactions to watch for so you can plan safely.
Simple, effective steps to quit
Pick a quit date and tell someone. People who say the date out loud and have support beat vague plans. Prepare for cravings by using nicotine replacement therapy (patches, gum, lozenges) or talking to your doctor about prescription options like bupropion or varenicline. Combining a medication with behavioral support or a quitline doubles your chance of success.
Change small daily habits: avoid places you smoked, replace the cigarette with a 3-minute walk, or use chewing gum or sunflower seeds when your hands want a cigarette. Use phone apps or text programs for reminders and tracking. If you slip, don’t treat it as failure—look for what triggered it and plan a different response next time.
How smoking changes medicines and why that matters
Smoking doesn’t just harm your lungs; it alters how your liver processes some drugs. Tobacco smoke induces an enzyme called CYP1A2. That speeds up removal of meds broken down by that enzyme, which can make them less effective. Examples include theophylline (for breathing), and some psychiatric medications such as clozapine and olanzapine.
When you quit, the enzyme activity drops and drug levels can rise suddenly. That can increase side effects unless doses are adjusted. Also, nicotine itself raises heart rate and blood pressure, so quitting changes cardiovascular load and can affect blood pressure meds. If you use hormonal contraception, smoking raises your risk of blood clots—especially if you’re over 35—so discuss safer options with your provider.
Tell every clinician you see that you smoke or recently stopped. They can check blood levels, reduce doses, or switch drugs when needed. This is especially important if you take heart medicines, seizure meds, psychiatric drugs, or strong painkillers.
Quick wins: within 20 minutes your pulse and blood pressure drop. After 12 hours carbon monoxide levels fall. In 2–12 weeks your circulation improves and lung function gets better. After 1 year your risk of heart disease is much lower, and over time many cancer risks go down too. These are real, measurable changes people notice.
If you want help, ask your doctor about nicotine replacement, bupropion, or varenicline, and use behavioral support. For medication changes, bring a list of everything you take—prescription, over-the-counter, and supplements—so your clinician can adjust safely. Quitting is one of the fastest ways to improve health, and planning around meds keeps the process safer and smoother.