Most people think hemorrhoids are just a minor annoyance - something you get if you sit too long or eat too little fiber. But here’s the truth: hemorrhoids are a common, often misunderstood condition that affects about 75% of people at some point in their lives. And while they’re rarely dangerous, they can be incredibly painful, embarrassing, and disruptive. The real issue isn’t just having them - it’s not knowing whether you’re dealing with internal or external hemorrhoids, and what to do next.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t some weird abnormality. They’re normal blood vessels - vascular cushions - that help you control bowel movements. Think of them like shock absorbers inside your anus and lower rectum. But when pressure builds up - from straining, pregnancy, constipation, or sitting too long - these veins swell, stretch, and irritate. That’s when they become a problem. There are two main types, and they’re not just different in location - they behave completely differently. The key difference? Pain.Internal Hemorrhoids: Silent but Not Harmless
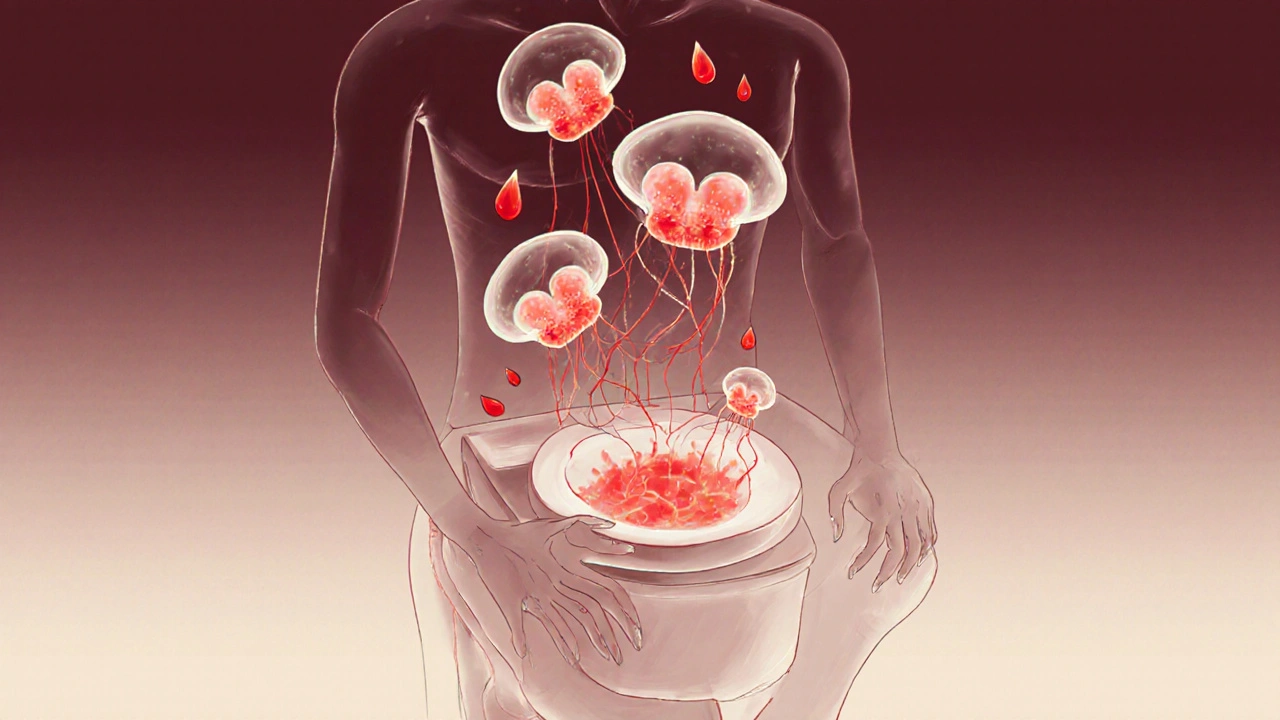
Internal hemorrhoids form inside the rectum, above a line called the dentate line. This area has no pain receptors, so even when they swell, you might not feel a thing. That’s why many people don’t realize they have them until they see bright red blood on the toilet paper or in the bowl after a bowel movement. Doctors grade internal hemorrhoids on a scale of I to IV:- Grade I: Just swollen. May bleed, but don’t prolapse (come out).
- Grade II: Prolapse during straining but pop back in on their own.
- Grade III: Come out and need to be pushed back in by hand.
- Grade IV: Stuck outside permanently. Can’t be pushed back.
External Hemorrhoids: The Painful Ones
External hemorrhoids form under the skin around the anus. This area is packed with nerves - which is why even a small bump can feel like a knife stab. You’ll likely notice:- A soft, skin-colored lump near the anus
- Itching or burning
- Pain when sitting or wiping
- Swelling that gets worse after bowel movements
Can You Have Both at Once?
Yes. And it’s more common than you think. Many people have a mix of internal and external hemorrhoids. That’s why symptoms can be confusing. You might have bleeding from inside (internal) and a painful lump outside (external). It’s easy to assume the pain is from the bleeding - but they’re two separate issues. That’s also why self-diagnosis fails. A lot of people think every anal itch or bit of blood is hemorrhoids. But anal fissures - tiny tears in the lining - also cause bleeding and pain. The difference? Fissures hurt like a sharp tear during bowel movements. Hemorrhoids cause more of a dull ache, pressure, or constant itch.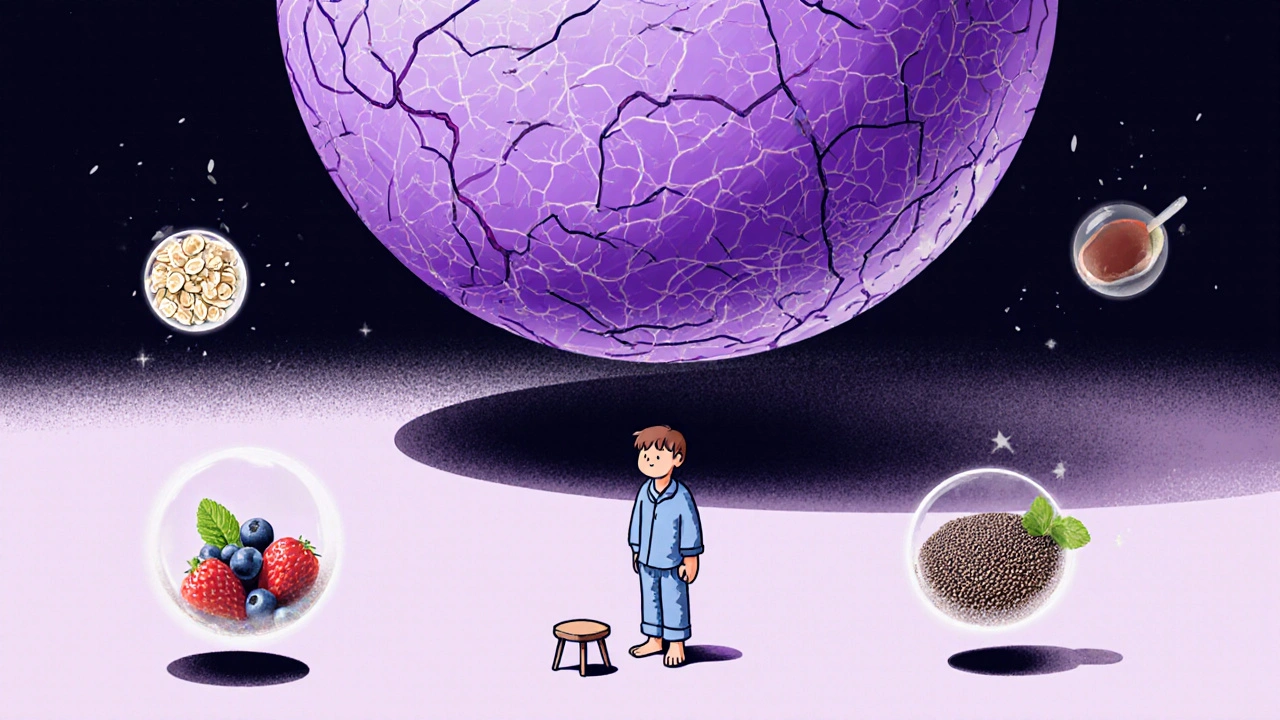
What Causes Hemorrhoids?
It’s not just bad diet or sitting too long. Here’s what actually triggers them:- Chronic constipation or diarrhea - both strain the rectal area
- Straining during bowel movements - even if it’s just a little
- Pregnancy - up to 35% of pregnant women get them, especially in the third trimester
- Obesity - extra weight increases pressure on pelvic veins
- Heavy lifting - especially with poor form
- Sitting for long periods - especially on the toilet
Treatment: What Actually Works
The good news? Most hemorrhoids get better with simple changes - no surgery needed.For Mild Cases: Home Care
- High-fiber diet: Aim for 25-30 grams of fiber daily. Think beans, oats, berries, broccoli, chia seeds. Most people get less than half that.
- Drink water: 8-10 glasses a day. Fiber without water just makes things worse.
- Sitz baths: Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Over-the-counter creams: Hydrocortisone cream for itching, witch hazel pads for inflammation. Avoid products with benzocaine or lidocaine long-term - they can irritate skin.
- Avoid straining: Don’t force a bowel movement. If it doesn’t come in 5 minutes, get up and try later.
For Internal Hemorrhoids: Minimally Invasive Procedures
If home care doesn’t work, doctors have tools that work fast and don’t require hospital stays:- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in a few days. It’s 90% effective for Grades I-III. You’ll feel pressure or mild cramping for 24-48 hours.
- Sclerotherapy: A chemical is injected into the hemorrhoid. It causes scarring and shrinkage. Less painful than bands, but slightly less effective.
- Infrared coagulation: Heat is applied to the tissue. It causes clotting and shrinkage. Good for smaller hemorrhoids.
For Thrombosed External Hemorrhoids
If you have a sudden, painful, purple lump - get seen within 72 hours. A simple procedure where the doctor makes a tiny cut and removes the clot can bring instant relief. Waiting longer means the clot hardens, and you’ll need to wait it out - which can take weeks.Surgery: Last Resort
If hemorrhoids keep coming back, or you have Grade IV prolapse, surgery may be needed:- Hemorrhoidectomy: The hemorrhoid is cut out. It’s the most effective - 95% success rate. But recovery takes 2-4 weeks. Pain is real. You’ll need prescription pain meds.
- Stapled hemorrhoidopexy: Used for prolapsed internal hemorrhoids. The surgeon staples the tissue back up. Less pain than removal, but higher chance of recurrence.
When to See a Doctor
Don’t wait until it’s unbearable. Call a doctor if:- Bleeding lasts more than a week or gets worse
- Pain doesn’t improve after a week of home care
- You feel dizzy, weak, or lightheaded - signs of significant blood loss
- Your bowel habits change - constipation turns to diarrhea, or vice versa
- You’re over 50 and have new rectal bleeding

Prevention: Stop the Cycle
The biggest mistake? Treating the symptom, not the cause. Even after surgery or ligation, if you keep straining, sitting too long, or eating low-fiber food - they’ll come back. Studies show:- People who stick to high fiber and hydration have only 5-10% recurrence
- Those who don’t? Up to 50% get them again
- Start your day with a high-fiber breakfast - oatmeal with flaxseed and berries
- Keep a water bottle with you. Sip all day.
- Move regularly. Even a 10-minute walk after meals helps digestion.
- Don’t read on the toilet. Limit bathroom time to 5 minutes max.
- If you’re pregnant, sleep on your left side. It takes pressure off your pelvic veins.
What Doesn’t Work
There’s a flood of “miracle cures” online: herbal creams, essential oil blends, “natural hemorrhoid removal kits.” Most are scams. The American Gastroenterological Association warns against them. They don’t fix the root problem - and some can burn or irritate sensitive tissue. And don’t rely on “just a little” bleeding. That’s your body’s warning sign. Ignore it, and it gets worse.Are hemorrhoids dangerous?
Hemorrhoids themselves aren’t dangerous, but they can cause complications like severe bleeding, infection, or tissue death if prolapsed and untreated. More importantly, rectal bleeding can be a sign of something more serious - like colorectal cancer. Never assume bleeding is just hemorrhoids without getting checked.
Can hemorrhoids go away on their own?
Mild cases, especially Grade I and II internal hemorrhoids, can shrink and improve with home care in a few days to a week. External hemorrhoids, especially if thrombosed, won’t go away without treatment - the clot may dissolve slowly, but the lump often stays. Prevention is key to avoid recurrence.
Is rubber band ligation painful?
Most people feel mild pressure or cramping for 1-2 days after the procedure. It’s not like surgery. You can usually return to work the next day. Pain is usually manageable with over-the-counter painkillers. The band falls off in 5-7 days, and the hemorrhoid shrinks.
Can I use wipes instead of toilet paper?
Avoid scented or alcohol-based wipes - they irritate the area. Use unscented, alcohol-free wipes or plain water. A bidet attachment or gentle rinse with warm water after bowel movements is better than wiping at all. Pat dry, don’t rub.
Do hemorrhoids increase cancer risk?
No. Hemorrhoids do not cause cancer. But they can mask cancer symptoms. That’s why anyone over 50 with new rectal bleeding should get a colon cancer screening. Don’t let hemorrhoids delay a necessary check-up.
Can I exercise with hemorrhoids?
Yes - but avoid heavy lifting or straining. Walking, swimming, and cycling are great. They improve circulation and prevent constipation. Avoid squats, deadlifts, or anything that forces you to hold your breath. If an exercise makes your hemorrhoids worse, stop and try something else.

Comments (7)
Pallab Dasgupta
Bro, I had a thrombosed external hemorrhoid last year and thought I was dying. Felt like a walnut had exploded in my butt. Went to urgent care and they just slit it open with a tiny knife-like, 30 seconds, no anesthesia, and instant relief. I cried. Not from pain-from shock that something so brutal could fix me so fast. Don’t wait. Just go.
Ellen Sales
People treat hemorrhoids like a personal failure-like you messed up your life and now your butt is punishing you. But it’s just anatomy. Your body’s trying to hold everything together under pressure. Fiber isn’t a chore-it’s a love letter to your colon. And sitting on the toilet scrolling TikTok? That’s not relaxation. That’s self-sabotage. Start small. One extra prune a day. One less minute on the bowl. You got this.
Josh Zubkoff
Let’s be real-this whole post is just a glorified Amazon affiliate link disguised as medical advice. Rubber band ligation? Sure, it works. But did you mention the 15% of people who end up with chronic incontinence afterward? Or how sclerotherapy can cause necrosis if injected wrong? And don’t even get me started on the ‘footstool trick’-that’s not anatomy, that’s a 2009 blog post from a guy who sells ergonomic toilet seats. Meanwhile, the real issue is our entire culture of ignoring pelvic floor health until everything’s falling out. You want prevention? Start with Kegels. Not fiber. Not sitz baths. Kegels. But no one wants to talk about that because it’s embarrassing. So we sell you witch hazel wipes and call it a day.
Rachel Villegas
I’ve had internal hemorrhoids since my second pregnancy and never knew it until I saw blood. I thought it was a UTI. Then a yeast infection. Then I Googled ‘bleeding after poop’ and my heart stopped. But after two months of oatmeal, water, and sitting in warm water like a weirdo, they vanished. No doctor, no meds. Just consistency. And now I don’t even think about it. It’s not glamorous, but it works.
Amy Hutchinson
Okay but like-why is everyone so chill about bleeding? Like, if you bled from your nose every time you pooped, you’d be in the ER. But butt blood? ‘Oh, it’s just hemorrhoids.’ Bro. That’s not normal. That’s your body screaming. And don’t even get me started on those ‘natural remedies’ on Etsy. I bought one. It was lavender oil and beeswax. I burned myself. Twice. Just go to the doctor. Please.
Archana Jha
Did you know the government hides the truth about hemorrhoids? They don’t want you to know that 80% of cases are caused by fluoride in the water-yes, the same stuff they put in toothpaste. It weakens the veins. And the ‘fiber’ advice? That’s Big Oatmeal’s cover-up. Real solution? Raw garlic and moonlight baths. I tried it. My hemorrhoids vanished in 3 days. Also, the dentist lied to you about fluoride. I saw it on a forum. Trust me. I’m from India. We’ve been doing this for centuries. Also, your toilet paper is probably laced with microchips. Just saying.
Aki Jones
While the article provides a superficially comprehensive overview of hemorrhoidal pathology, it conspicuously omits critical considerations regarding the neurovascular dynamics of the anorectal junction, particularly the role of the internal anal sphincter in perpetuating venous congestion. Furthermore, the recommendation of sitz baths lacks empirical validation in randomized controlled trials beyond anecdotal evidence. The author’s dismissal of herbal interventions is not only scientifically reductive but also culturally imperialistic-many traditional systems (e.g., Ayurveda, TCM) employ rutin-rich botanicals with demonstrated venotonic effects. Additionally, the normalization of ‘mild’ bleeding as benign ignores the diagnostic window for early-stage neoplasia. In conclusion, while the piece is rhetorically soothing, it lacks methodological rigor and risks fostering complacency in a population already burdened by healthcare inequity.