Polydipsia treatment: practical steps to manage constant thirst
Always thirsty? That constant need to drink has a name: polydipsia. It can come from simple habits or serious medical conditions. The good news is treatment usually works once you know the cause. Here’s a clear, practical plan to help you or someone you care about feel normal again.
Quick check: what might be causing your thirst
Start by thinking through the basics. High blood sugar from uncontrolled diabetes mellitus makes you pee more and drives thirst. Diabetes insipidus (DI) — either central or nephrogenic — prevents your kidneys from concentrating urine, so you lose water fast. Psychogenic (primary) polydipsia is drinking too much out of habit or stress. Less common causes include certain medications (diuretics, lithium), kidney problems, and rare endocrine issues.
How doctors figure it out
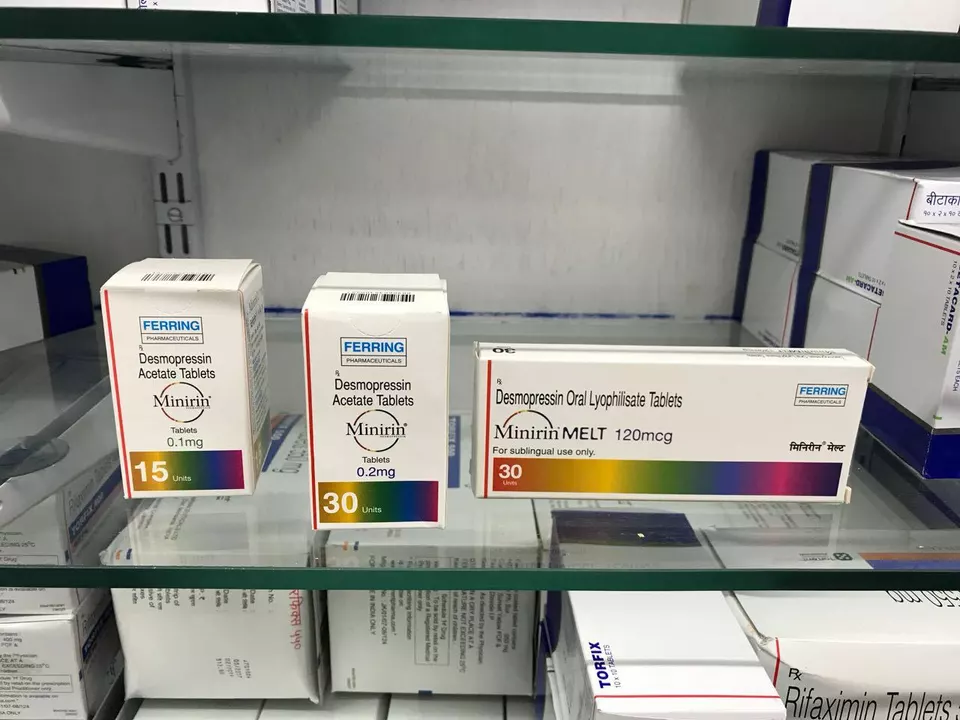
Your healthcare provider will want a few simple tests first: fasting blood glucose, serum sodium, and basic kidney work. A large urine volume or low urine osmolality points to DI or excessive drinking. If results aren’t clear, a water-deprivation test or a desmopressin (DDAVP) challenge can separate central DI, nephrogenic DI, and primary polydipsia. Don’t try a dehydration test at home — it can be risky.
Treatment targets the cause. If high blood sugar is driving thirst, controlling diabetes with diet, medications, and monitoring will reduce thirst quickly. For central DI, desmopressin replaces the missing hormone and cuts thirst and urine output. For nephrogenic DI, doctors focus on low-sodium diet, thiazide diuretics, and sometimes NSAIDs to help the kidneys hold water better. If a drug is causing the problem, stopping or switching that medicine may fix it.
Psychogenic polydipsia needs a different approach. Behavioral strategies like scheduled fluids, working with a therapist, and treating underlying anxiety or psychosis work best. In severe cases, supervised fluid restriction and close monitoring of sodium levels are required because sudden changes can cause dangerous imbalances.
Safety matters. Drinking too much water can lead to hyponatremia — low blood sodium — which causes headache, nausea, confusion, seizures, or worse. If you or someone else shows confusion, severe headache, vomiting, seizure, or loss of consciousness, get emergency care.
Practical tips you can start today: keep a daily log of fluids and urine frequency for a few days, check blood sugar if you have risk factors for diabetes, avoid unlimited water challenges, and bring your notes to your appointment. Small changes — cutting down caffeinated diuretics, managing medications, or getting blood tests — often points the way to the right treatment.
Treatment is usually straightforward once the cause is known. Work closely with your doctor, follow testing safely, and watch for warning signs. With the right plan, that constant thirst can become a problem of the past.