Understanding Polydipsia and Its Impact on Patients
Before we delve into the use of desmopressin for the treatment of polydipsia, it is essential to understand what polydipsia is and how it affects patients. Polydipsia is a condition characterized by excessive thirst and fluid intake, often resulting in the consumption of large amounts of water. This can lead to a variety of health issues, such as electrolyte imbalances, kidney problems, and even mental confusion.
The exact cause of polydipsia is not always clear, but it can be associated with certain medical conditions, such as diabetes insipidus and psychogenic polydipsia. It is crucial to identify and address the underlying cause to ensure proper treatment and management of the condition. In this article, we will explore the role of desmopressin in managing polydipsia and improving the quality of life for patients experiencing this challenging condition.
Desmopressin: An Overview of Its Mechanism of Action
Desmopressin is a synthetic form of the hormone vasopressin, which plays a vital role in regulating the balance of water in the body. Vasopressin, also known as antidiuretic hormone (ADH), is produced by the hypothalamus and released by the posterior pituitary gland. It acts on the kidneys to reduce the amount of water excreted in the urine, thereby helping to maintain proper hydration and electrolyte balance.
Desmopressin works by mimicking the effects of natural vasopressin, binding to specific receptors in the kidneys and promoting the reabsorption of water. This leads to a decrease in urine production and helps to alleviate the symptoms of polydipsia. It is important to note that desmopressin does not address the root cause of polydipsia, but rather helps to manage the symptoms and reduce the risk of complications associated with excessive water intake.
Using Desmopressin for the Treatment of Polydipsia: Dosage and Administration
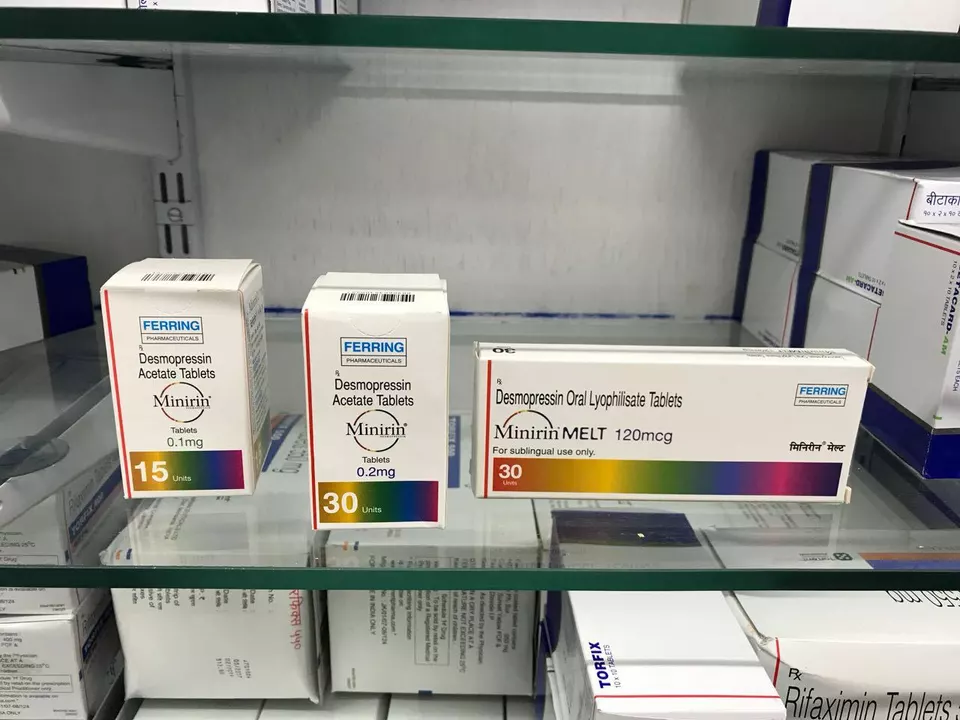
Desmopressin is available in various forms, including tablets, nasal spray, and injectable solutions. It is important to follow your healthcare provider's instructions and recommendations when using desmopressin to ensure optimal results and minimize the risk of side effects. The dosage and administration of desmopressin may vary depending on the patient's age, weight, and specific medical condition.
In general, the starting dose of desmopressin for the treatment of polydipsia is relatively low, with adjustments made based on the patient's response to the medication. It is crucial to monitor urine output and electrolyte levels while using desmopressin to ensure proper hydration and avoid complications such as hyponatremia (low sodium levels in the blood). Your healthcare provider may also recommend additional tests or adjustments to your treatment regimen to optimize the effectiveness of desmopressin and ensure your safety.
Potential Side Effects and Risks Associated with Desmopressin Use
As with any medication, there are potential side effects and risks associated with the use of desmopressin. Some of the most common side effects include headache, nausea, abdominal pain, and mild nasal congestion (if using the nasal spray form). These side effects are generally mild and resolve on their own as your body adjusts to the medication.
More serious side effects and risks associated with desmopressin use include hyponatremia, water intoxication, and allergic reactions. Hyponatremia, in particular, can be life-threatening if not promptly identified and treated, as it can lead to seizures, coma, and even death. It is crucial to monitor your fluid intake and receive regular blood tests to assess your electrolyte levels while using desmopressin. If you experience any signs of hyponatremia, such as headache, nausea, vomiting, muscle cramps, or confusion, contact your healthcare provider immediately.
Additional Tips for Managing Polydipsia and Maintaining a Healthy Lifestyle
While desmopressin can be an effective treatment option for managing the symptoms of polydipsia, it is important to also address the underlying cause and make necessary lifestyle adjustments to ensure optimal health and well-being. This may include working with your healthcare provider to identify and treat any underlying medical conditions or seeking counseling for psychological factors contributing to excessive thirst and water intake.
In addition to using desmopressin, maintaining a healthy diet and staying active can also help manage polydipsia and improve your overall quality of life. Consuming foods rich in electrolytes, such as fruits, vegetables, and whole grains, can help maintain proper hydration and electrolyte balance. Engaging in regular physical activity can also help regulate fluid levels in the body and promote overall health. Be sure to consult with your healthcare provider before making any significant changes to your diet or exercise routine to ensure they are safe and appropriate for your specific needs.

Comments (20)
Pat Mills
Desmopressin may look like a miracle drug, but the truth is buried beneath layers of pharmaceutical hype.
As an American who champions evidence‑based medicine, I demand rigorous data before we start prescribing it en masse.
The studies cited in the guide often involve tiny cohorts that hardly represent our diverse population.
Moreover, the authors conveniently downplay the risk of hyponatremia, a condition that can cripple even a healthy individual.
When you flood the body with an antidiuretic hormone analogue, you tangle yourself in a web of fluid overload.
Patients with psychogenic polydipsia are especially vulnerable because their thirst drive is already dysregulated.
Imagine adding a synthetic ADH on top of that – the outcome can be catastrophic.
The guide also neglects to mention the cost burden on the healthcare system, a factor that cannot be ignored.
We must ask ourselves whether a cheap nasal spray truly outweighs the potential for life‑threatening seizures.
In my view, behavioral therapy and proper monitoring of fluid intake should be the first line of defense.
Only after those avenues are exhausted should we even contemplate desmopressin.
Unfortunately, the article glosses over this hierarchy, presenting the drug as a silver bullet.
The dramatic language used throughout feels like a sales pitch rather than a balanced medical review.
I am proud of America's commitment to patient safety, and that means demanding transparency.
If researchers want to win the trust of clinicians, they must publish raw data and long‑term follow‑up.
Until then, I remain skeptical and advise my colleagues to tread carefully.
neethu Sreenivas
Reading through this guide, I couldn't help but reflect on how our thirst for quick fixes mirrors deeper existential cravings.
It's a reminder that sometimes the body signals a deeper imbalance that medication alone can't soothe.
We must listen with compassion, both to the physiological cues and the emotional undercurrents driving them.
Balancing science with humanity is the true art of healing 😊🌿.
Keli Richards
Interesting overview but I wish there were more real‑world examples it feels a bit textbook.
Ravikumar Padala
Well, I skimmed the whole thing and honestly it reads like a marketing brochure written by a sleep‑deprived intern.
The sections on mechanism of action are vague and the dosage tables seem copied from a generic drug label without any nuance for individual patient scenarios.
While the author tries to sound authoritative, the lack of discussion about long‑term monitoring makes me wonder if they even considered real clinical practice.
Overall, it's a decent primer if you're new to the topic but not something you'd cite in a serious discussion.
King Shayne I
Look, this guide is oversellin desmopressin like it's a cure‑all, and that's just plain wrong. The side effects are real and the author doesn't even mention proper patient selection. Get your facts straight before you push this drug on anyone.
jennifer jackson
Stay hopeful and keep sipping smartly!
Brenda Martinez
The guide's enthusiasm for desmopressin borders on theatrical-almost as if the author wants us to applaud the drug's entrance on stage.
Yet the reality is far less glamorous; the risk of hyponatremia is a silent antagonist that can crash the performance.
People with psychogenic polydipsia already dance on the edge of fluid imbalance, and adding a synthetic hormone can be a fatal misstep.
Moreover, the dosage recommendations feel like a one‑size‑fits‑all costume, ignoring the nuanced choreography each patient requires.
While the article touts improved quality of life, it neglects to acknowledge the psychological burden of constant monitoring.
In my experience, the best outcomes arise from multidisciplinary approaches, not a single pharmacologic hero.
Thus, this guide, though comprehensive in length, fails to deliver a balanced script for clinicians.
Marlene Schanz
hey folks, just wanted to add a quick note-if you're considering desmopressin, make sure to check electrolytes regularly. I've seen a couple of cases where patients got a bit too water‑locked and ended up with low sodium. Also, keep an eye on blood pressure; sometimes the nasal spray can cause a mild rise. Stay safe!
Matthew Ulvik
Great summary! 👍 If anyone's new to this, start with low doses and monitor urine output. Always keep a water‑intake log, it helps a lot.
Dharmendra Singh
In reviewing desmopressin's role, it's vital to contextualize it within cultural practices around fluid consumption. Some Communities emphasize high water intake for health, which can complicate dosing. Ensure that patient education respects these traditions while highlighting the need for monitoring.
Rocco Abel
One must approach the discourse on desmopressin with a measured skepticism befitting a scholar of the highest order.
It is not merely a pharmacologic agent but a symbol of the vast, often concealed machinations within the pharmaceutical complex.
The literature, when scrutinized through a lens honed by years of rigorous inquiry, reveals an unsettling pattern of selective reporting.
Thus, the clinician, ever vigilant, must dissect each claim with a scalpel of analytical precision, lest we be seduced by the siren song of convenience.
Dawn Mich
Don't be fooled by the polished language-this is part of a larger agenda to push unnecessary drugs onto patients.
The side‑effect profile is intentionally downplayed, and the supposed benefits are overstated to create demand.
Eric Sevigny
While the guide covers the basics, it could benefit from a deeper dive into monitoring protocols.
I've noticed that clinicians often overlook the subtle signs of hyponatremia, which can be mitigated with regular labs.
Glenda Rosa
Ah, another megalithic endorsement of desmopressin-how utterly predictable! One would think the authors have uncovered the elixir of eternal hydration, yet they gloss over the perilous waters of electrolyte chaos. It's a beautifully crafted catastrophe dressed in clinical prose.
charlise webster
Not all patients need desmopressin; lifestyle changes often suffice.
lata Kide
🚨🚨 Listen up, everyone! 🚨🚨 This guide tries to sell desmopressin like it's a miracle, but the reality is a ticking time bomb of water intoxication! 😱💦 If you don't monitor electrolytes, you're playing Russian roulette with your kidneys! 💀💉 The drama isn't just in the text-it’s in the lives of patients who might suffer severe hyponatremia! 😡 So, before you jump on the bandwagon, read the fine print, stay vigilant, and protect your health! 🌟🙌
Mark Eddinger
The article provides a solid foundation; however, clinicians should also consider the patient's baseline renal function when initiating therapy.
Francisco Garcia
Thanks for the thorough overview! I'm curious about the real‑world adherence rates-do patients actually stay on desmopressin long‑term, or do they drop off due to side effects? Also, any tips on integrating behavioral interventions alongside medication would be appreciated.
Patrick Renneker
While the essay exalts desmopressin's pharmacodynamics, it neglects to address the profound ethical implications of prescribing a hormone analog without exhaustive longitudinal data.
The author’s reliance on limited trials appears to be an oversimplification that undermines the complexity inherent in managing polydipsia.
Consequently, practitioners ought to adopt a more circumspect stance, privileging patient safety above expedient therapeutic trends.
KAYLEE MCDONALD
Take the medication only if your doctor monitors electrolytes closely; safety first.