Desmopressin: What it does and how to use it safely
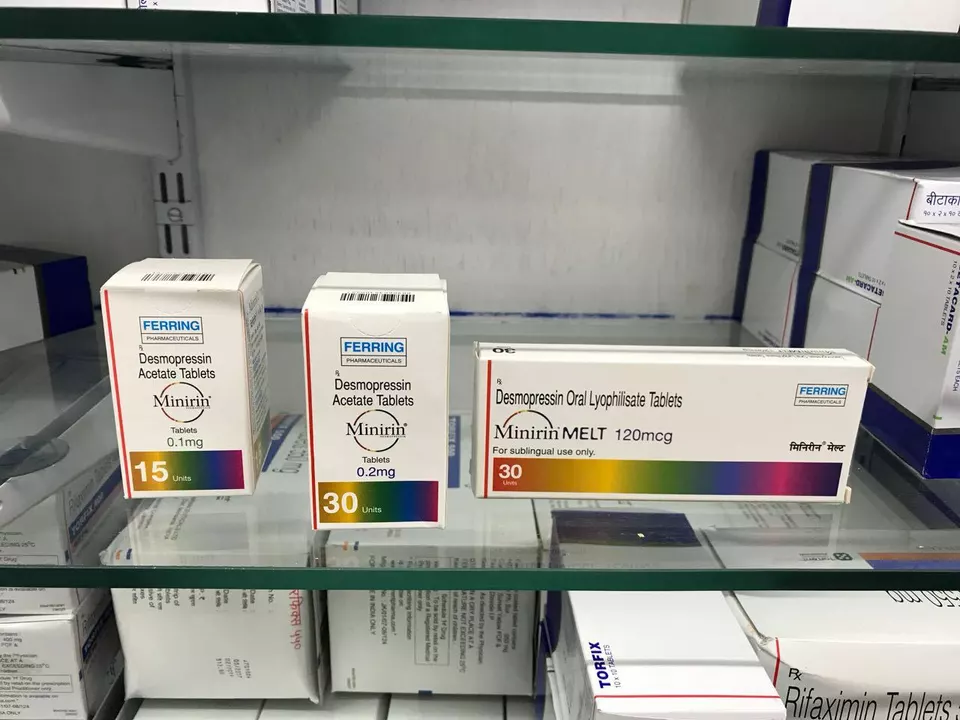
Desmopressin is a medicine that lowers urine production and can also raise some clotting factors for certain bleeding problems. People take it for central diabetes insipidus (when the body can’t concentrate urine), for bedwetting at night, for bothersome nocturia, and sometimes before minor procedures to reduce bleeding in patients with mild von Willebrand disease. It comes as tablets, an oral melt, a nasal spray, and as an injection. Each form acts the same way in the body but has different dosing and practical rules.
Common uses and what typical dosing looks like
For diabetes insipidus doctors usually start low and adjust. Patients might begin on small oral doses such as 0.05 mg two to three times a day and change from there based on urine output and blood sodium. For bedwetting, a single bedtime dose is common: adults and children often use 0.1–0.2 mg orally at night or the manufacturer’s recommended oral melt dose. For nocturia a single low dose at bedtime may cut down nighttime bathroom trips. When used to prepare for minor surgery in bleeding disorders, desmopressin is typically given by injection or intranasal spray under medical supervision; a common IV dose for that use is about 0.3 mcg per kg given once, but your hematologist will decide the right plan. Dosing depends on age, weight, kidney function, and the exact reason for treatment, so always follow the prescriber’s instructions.
Safety, side effects, and practical tips
The biggest safety issue is low blood sodium, called hyponatremia. Desmopressin reduces how much water the kidneys let go, so drinking a lot of fluid while on it can dangerously dilute sodium. Doctors often ask patients to limit fluids around the time they take the dose and to check blood sodium before treatment and after starting or changing the dose. Watch for headache, nausea, confusion, weakness, or seizures — these can be signs of low sodium.
Common side effects include mild headache, nausea, nasal irritation with the spray, and dizziness. Serious fluid overload and severe hyponatremia are less common but require quick medical attention. Tell your prescriber about other medicines that increase hyponatremia risk, like thiazide diuretics, some antidepressants (SSRIs or tricyclics), carbamazepine, or recent surgery or illness. Older adults and people with heart or kidney disease need closer monitoring.
Practical tips: don’t swap formulations on your own — the dose numbers don’t match across tablets, melts, spray, and injection. If you use the nasal spray, avoid blowing your nose right before or after dosing. Never double a missed dose; follow your clinician’s instruction. Store the product as the leaflet says, and check expiry dates. If you’re pregnant, breastfeeding, or planning surgery, mention desmopressin to every clinician involved in your care.
Call your doctor if you get severe headache, vomiting, sudden swelling, confusion, or seizures. Ask about how often to check sodium, any fluid limits to follow, and whether desmopressin is the best choice for you. Used correctly and with basic monitoring, desmopressin can work very well, but attention to fluids and interactions matters more than you might expect.