When you’re prescribed a blood‑pressure pill, the last thing you want to worry about is a sudden flare‑up of joint pain. Yet a surprising number of patients on the popular combo drug Lisinopril‑HCTZ is a fixed‑dose blend of the ACE inhibitor lisinopril and the thiazide diuretic hydrochlorothiazide used to control hypertension report gout attacks. Understanding why this happens, how big the risk really is, and what you can do about it turns a confusing side‑effect into an actionable plan.
Key Takeaways
- Thiazide diuretics raise blood uric acid, which can trigger gout in susceptible people.
- ACE inhibitors like lisinopril have a neutral or slightly protective effect on uric‑acid levels.
- The overall gout risk for Lisinopril‑HCTZ sits between that of pure thiazides and pure ACE inhibitors.
- Monitoring serum uric‑acid and kidney function can catch problems early.
- Diet tweaks, lifestyle changes, or a switch to a different antihypertensive often prevent recurrent attacks.
What Is Gout?
Gout is a form of inflammatory arthritis caused by the deposition of monosodium urate crystals in joints and soft tissue. The culprit is elevated uric acid in the blood, which can exceed its solubility limit and crystallise, most often in the big toe but also in knees, ankles and hands.
Typical symptoms include sudden, intense pain, swelling, redness and warmth. If untreated, gout can become chronic, leading to joint damage and tophi-hard nodules of urate crystals under the skin.
Why Blood‑Pressure Pills Matter
High blood pressure (or hypertension is a chronic condition where the force of blood against artery walls is consistently too high) is a leading driver of heart attacks and stroke. Doctors often reach for a combination pill because it simplifies dosing, improves adherence, and tackles two pathways at once: the renin‑angiotensin system (via lisinopril) and sodium‑water retention (via hydrochlorothiazide).
But the diuretic half of the equation-hydrochlorothiazide is a thiazide‑type diuretic that promotes urine output by inhibiting sodium‑chloride transport in the distal convoluted tubule-has a well‑documented side‑effect profile that includes raising serum uric‑acid levels. This is where gout risk enters the picture.
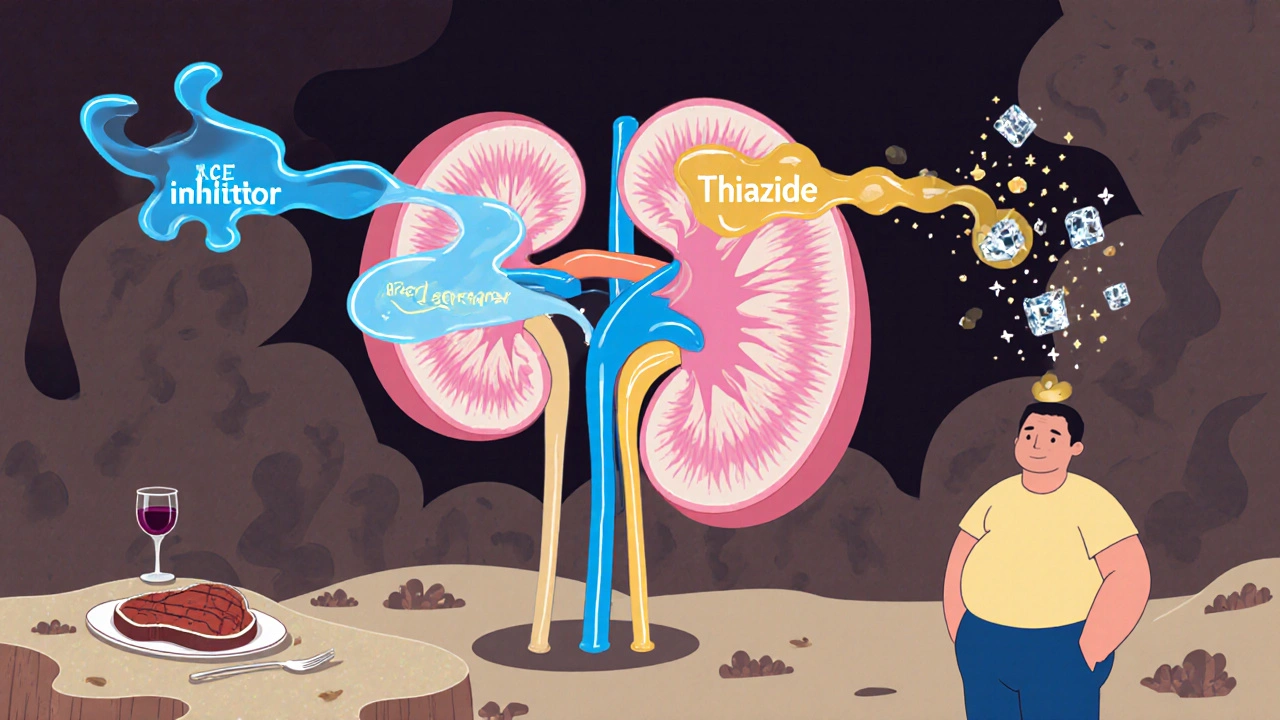
How the Lisinopril‑HCTZ Combo Influences Uric‑Acid
Two mechanisms are at play:
- Thiazide‑induced urate reabsorption: Thiazides increase sodium loss, which the kidney compensates for by reabsorbing more urate in the proximal tubule. The net effect is higher serum uric‑acid.
- ACE‑inhibitor effect: Lisinopril, an ACE inhibitor is a drug that blocks the conversion of angiotensin I to angiotensin II, lowering blood pressure, appears to have a neutral or modestly uric‑acid‑lowering effect, possibly through improved renal perfusion.
When you combine them, the thiazide’s urate‑raising impact is partially offset by the ACE inhibitor, placing the overall risk somewhere between that of a pure thiazide (higher risk) and a pure ACE inhibitor (low risk). Clinical studies from 2018‑2023 report a 1.5‑ to 2‑fold increase in gout incidence among patients on Lisinopril‑HCTZ compared with lisinopril alone.
Who Is Most Vulnerable?
Not everyone on Lisinopril‑HCTZ will develop gout. The biggest predictors are:
- Baseline serum uric‑acid >6.8 mg/dL
- Existing chronic kidney disease (CKD) - reduced kidney function is the ability of the kidneys to filter waste and maintain electrolyte balance hampers uric‑acid excretion.
- Male sex, especially over 40, because normal uric‑acid levels are higher in men.
- Obesity, high‑purine diet (red meat, seafood, alcohol)
- Use of other uric‑acid‑raising drugs (low‑dose aspirin, cyclosporine).
If you fall into one or more of these categories, keep a closer eye on your labs and symptoms.
Monitoring: Labs & Symptoms
Guidelines suggest checking serum uric‑acid and creatinine at baseline, then 4‑6 weeks after starting Lisinopril‑HCTZ, and yearly thereafter. A rise of more than 1 mg/dL or a value crossing the 7 mg/dL threshold warrants action.
Watch for classic gout flags: sudden onset pain in the big toe (podagra), swelling of the ankle or knee, or a feeling of “burning” after a high‑purine meal. Early treatment with colchicine or NSAIDs can abort an attack and minimise joint damage.
Managing the Risk
There are three practical pathways you can take:
- Maintain the combo but control uric‑acid: Add a urate‑lowering drug such as allopurinol is a xanthine oxidase inhibitor that reduces uric‑acid production. Start at 100 mg daily, titrate based on serum levels. Lifestyle tweaks-hydration, limiting alcohol and purine‑rich foods-also help.
- Swap the thiazide component: Replace hydrochlorothiazide with a potassium‑sparing diuretic (e.g., spironolactone) or an ACE inhibitor/ARB alone. Studies show a 30‑40 % drop in gout incidence after the switch.
- Switch to a different antihypertensive class: Calcium‑channel blockers (amlodipine), ARBs (losartan), or newer combos (olmesartan‑hydrochlorothiazide) have a more favourable uric‑acid profile.
The choice depends on your overall cardiovascular risk, kidney health, and how well you tolerate alternatives.

Comparison of Common Antihypertensives and Gout Risk
| Drug / Combo | Mechanism | Typical Dose | Gout Risk |
|---|---|---|---|
| Lisinopril‑HCTZ | ACE inhibitor + Thiazide diuretic | 10‑40 mg / 12.5‑25 mg | Moderate (↑ uric‑acid) |
| Lisinopril alone | ACE inhibitor | 10‑40 mg | Low (neutral) |
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑50 mg | High (↑ uric‑acid) |
| Losartan | ARB | 50‑100 mg | Low‑to‑moderate (may lower uric‑acid) |
| Amlodipine | Calcium‑channel blocker | 5‑10 mg | Low (no effect) |
Notice that the only drug consistently linked to a rise in uric‑acid is the thiazide. Pairing it with an ACE inhibitor blunts the spike but does not erase it.
Practical Tips to Reduce Gout Flares While on Lisinopril‑HCTZ
- Drink at least 2‑3 L of water daily; hydration helps flush uric‑acid.
- Limit purine‑rich foods: red meat, organ meats, sardines, anchovies.
- Cut sugary drinks and high‑fructose corn syrup-both raise uric‑acid.
- Avoid alcohol, especially beer and spirits, during flare‑prone periods.
- Maintain a healthy weight; each kilogram lost can drop uric‑acid ~0.1 mg/dL.
- Discuss with your doctor the possibility of adding Lisinopril HCTZ gout prophylaxis (low‑dose colchicine or allopurinol) if you have recurring attacks.
When to Call Your Healthcare Provider
If you experience any of the following, seek medical advice promptly:
- Joint pain lasting more than 24 hours or worsening despite over‑the‑counter NSAIDs.
- Fever, chills, or swelling that spreads to multiple joints.
- New‑onset kidney pain, decreased urine output, or unexplained fatigue-possible sign of worsening renal function.
- Laboratory results showing uric‑acid >9 mg/dL or a rapid rise.
Early intervention can prevent chronic gout and protect kidney health.
Bottom Line
While the Lisinopril‑HCTZ combo is an effective, once‑daily solution for hypertension, its thiazide component can nudge uric‑acid upward and trigger gout in susceptible individuals. By staying vigilant-monitoring labs, recognizing symptoms, and working with your clinician on drug choices or adjunctive urate‑lowering therapy-you can keep blood pressure under control without paying the price of painful joint attacks.
Does Lisinopril‑HCTZ cause gout in everyone?
No. Only people who already have risk factors-high baseline uric‑acid, kidney disease, obesity, or a genetic propensity-are likely to develop gout while on the medication.
Can I keep taking Lisinopril‑HCTZ if I get a gout flare?
Often yes, but you should discuss it with your doctor. They may add a urate‑lowering drug, adjust the dose, or switch the thiazide part to a different diuretic.
What lab values should I track?
Baseline and follow‑up serum uric‑acid, serum creatinine (or eGFR) to gauge kidney function, and electrolytes (especially potassium) are the key values.
Is there a safer blood‑pressure alternative for gout‑prone patients?
Yes. Options like losartan, amlodipine, or a lisinopril‑only regimen avoid the thiazide‑induced uric‑acid rise and are widely used.
How quickly can a gout attack be stopped?
Starting colchicine, high‑dose NSAIDs, or a corticosteroid within the first 24 hours can often halt the pain within a day. Delayed treatment may prolong the flare.


Comments (12)
cariletta jones
If you have a family history of gout, keep an eye on your uric‑acid levels while on Lisinopril‑HCTZ – a quick blood test every few months can catch spikes early.
Kevin Hylant
Don’t ignore a sudden toe pain; it’s often gout. Stop the flare fast with NSAIDs or colchicine and tell your doctor to check your meds.
Eileen Peck
i totally get how confusing this combo can be, especially when you’re trying to juggle blood pressure and joint pain. the good news is that most docs will happily switch you to a potassium‑sparring diuretic if uric‑acid climbs. also, staying well‑hydrated and cutting back on beer can make a big difference. remember, the key is regular labs – you’ll spot problems before they become full‑blown attacks.
Jonathan Harmeling
It’s a shame that some people ignore the science and keep taking a drug that literally spikes uric‑acid, putting their joints at risk. We have a duty to follow evidence‑based guidelines, not just chase lower blood pressure numbers. Let’s be honest, health is a package deal, not a trade‑off.
Ritik Chaurasia
Listen, the Indian community often relies on traditional diets that are already low in purines, so adding a thiazide can tip the balance dramatically. Drop the extra salt and switch to a safer antihypertensive before your knees start screaming.
Steven Young
They don’t tell you that big pharma designs these combos to keep you dependent, the hidden uric‑acid rise is just another profit engine. Keep your eyes open.
Kelly Brammer
Following the recommended monitoring schedule is not optional; it’s a moral responsibility to yourself and your family. Skipping labs shows a lack of respect for the very guidelines that keep us safe.
Ben Collins
Sure, because adding another pill is the *perfect* solution.
Denver Bright
I’ve been on Lisinopril‑HCTZ for a year and noticed occasional ankle swelling that turned out to be mild gout. It wasn’t severe, but I did end up talking to my doctor about swapping the thiazide. The switch made my joints feel a lot calmer.
Kelli Benedik
OMG, I literally felt like my toe was on fire 🔥 and I was like “no way am I letting this ruin my day!” 😱 Then I googled and found out it was the HCTZ sneaking uric‑acid up. Thank goodness I talked to my doc and got switched – crisis averted! 🙌
Marrisa Moccasin
Did you know that the “neutral” stance on uric‑acid is often a cover‑up, a deliberate distraction, a way to keep patients from questioning the combo’s true impact? The evidence is there, hidden in fine‑print, and it points to a real risk, not a myth.
Caleb Clark
Alright, let’s break this down step by step so you can feel confident managing both your blood pressure and your gout risk. First, schedule a baseline uric‑acid test before you start or continue the Lisinopril‑HCTZ combo – that gives you a reference point. Second, set a reminder for a follow‑up lab at 4‑6 weeks; if you see a jump of more than 1 mg/dL, that’s a red flag. Third, keep a simple journal of any joint pain, noting the day, the location, and what you ate that day; patterns often emerge with purine‑rich meals or alcohol. Fourth, stay diligent about hydration – aim for at least 2‑3 liters of water daily, which helps flush excess uric acid. Fifth, consider a modest diet tweak: reduce red meat, organ meats, and sugary drinks, which are known culprits. Sixth, if you have a history of kidney issues, discuss with your physician the possibility of swapping the thiazide for a potassium‑sparing diuretic or an ARB like losartan, which can actually lower uric acid. Seventh, don’t forget the power of a low‑dose colchicine prophylaxis if you’ve had more than one flare; it’s proven to keep attacks at bay. Eighth, when a flare does happen, act fast – NSAIDs, colchicine, or a short course of steroids can stop the pain within 24 hours if started early. Ninth, keep your medication list up to date in a health app so your pharmacist can spot drug interactions that might worsen gout. Tenth, involve a pharmacist in the conversation; they often have practical tips on timing doses to minimize uric‑acid spikes. Eleventh, if you’re on allopurinol, make sure the dose is titrated correctly – too low won’t help, too high can cause adverse effects. Twelfth, remember that stress can indirectly raise uric‑acid levels, so incorporate gentle exercise like walking or yoga into your routine. Thirteenth, regular check‑ins with your primary care provider are essential; they can adjust dosages based on the latest labs. Fourteenth, if you ever feel overwhelmed, reach out to a support group for hypertension or gout patients – shared experiences are empowering. Finally, stay optimistic: by monitoring, tweaking lifestyle, and collaborating with your healthcare team, you can keep both your blood pressure and joints in the green zone.