Medication Safety Checklist Tool
Medication Safety Verification
Verify each step of medication administration using the 5 rights plus critical additional safety checks from the latest guidelines
Safety Checklist
Safety Assessment
How to Use
Enter medication details and complete the checklist. Click 'Verify Safety' to assess risk and receive personalized recommendations based on the latest safety guidelines.
Recommended safety actions will appear here after verification
Medication errors kill more people than car accidents in the U.S. every year.
That’s not a hypothetical. It’s a fact backed by the Agency for Healthcare Research and Quality: over 7,000 deaths annually stem from preventable mistakes in prescribing, dispensing, or giving medications. And it’s not just hospitals-primary care clinics, nursing homes, and even telehealth visits are at risk. The problem isn’t bad people. It’s broken systems, tired staff, and technology that doesn’t always help.
But here’s the good news: we know how to fix it. The tools, training, and protocols exist. What’s missing is consistent, real-world application. For healthcare providers, medication safety isn’t just a policy-it’s the line between life and death.
What Medication Safety Really Means
Medication safety isn’t about avoiding mistakes. It’s about designing systems so mistakes don’t happen-or don’t hurt patients when they do.
The World Health Organization defines it as ensuring patients get the right drug, in the right dose, at the right time, through the right route-without harm. Sounds simple. But in practice, it’s a chain of 12+ steps: prescribing, transcribing, dispensing, administering, monitoring. One slip anywhere, and someone could die.
Take methotrexate. Used for cancer and autoimmune diseases. A patient gets it daily instead of weekly? That’s often fatal. In 2020, the Institute for Safe Medication Practices (ISMP) made it a hard stop in electronic systems: if a doctor orders daily methotrexate, the system won’t let them proceed unless they confirm it’s for cancer treatment. That’s medication safety in action.
High-alert medications like IV oxytocin, insulin, and heparin are the biggest risks. They’re powerful. Small errors cause big harm. That’s why hospitals now require double-checks, specialized protocols, and mandatory training before staff can handle them.
The Five Rights-And Why They’re Not Enough
You’ve heard them: right patient, right drug, right dose, right route, right time. They’re the foundation. But they’re also the bare minimum.
Barcode-assisted medication administration (BCMA) was supposed to solve this. Nurses scan the patient’s wristband, the drug, and the syringe. If it doesn’t match, the system stops them. Studies show BCMA cuts administration errors by 41%. Sounds perfect.
But here’s what no one talks about: workarounds.
On the floor, during a code blue or a rushed shift, nurses bypass the scanner. They’re tired. The system is slow. The barcode is smudged. So they override it. One study found 68% of nurses admit to bypassing BCMA in emergencies. That’s not defiance-it’s survival. And it’s dangerous.
So the real question isn’t whether BCMA works. It’s: how do we make it work without making staff feel like they’re fighting the system?
Technology Helps-Until It Doesn’t
Electronic health records (EHRs) and clinical decision support (CDS) systems were supposed to be the saviors. They flag drug interactions, duplicate orders, wrong doses. But here’s the catch: they flag too much.
Studies show clinicians override 49% to 96% of alerts. Why? Because 90% of them are noise. A 72-year-old with high blood pressure gets a warning about a drug interaction with a supplement they stopped taking three years ago. You see it once-it’s helpful. You see it 20 times a shift? You start clicking ‘ignore’ without reading.
Alert fatigue is real. And it’s killing people.
Worse, EHRs create new errors. A 2021 study from Brigham and Women’s Hospital found 34% of digital medication errors came from default settings. A doctor selects ‘30 mg’ because that’s the default for a common drug-but the patient needs 15 mg. They don’t notice. The system doesn’t make it obvious.
Technology isn’t the problem. Poor design is.

Training That Actually Works
Most hospitals give new hires a 2-hour PowerPoint on medication safety. Then they’re thrown into the ER. That’s not training. That’s negligence.
The Agency for Healthcare Research and Quality (AHRQ) recommends 16 to 24 hours of initial training-plus 8 hours every year. And it has to be hands-on.
Simulation labs are the gold standard. Nurses practice giving insulin to a mannequin with a glucose monitor that drops dangerously low if they get the dose wrong. Pharmacists role-play with doctors about a confusing order. Teams debrief after every error-even near-misses.
At Johns Hopkins, embedding pharmacists in ICU units cut medication errors by 81%. Why? Because someone with drug expertise was there, in real time, asking questions before the med went in.
Training isn’t about memorizing rules. It’s about building habits. And habits take practice, feedback, and repetition.
Culture Is the Secret Weapon
Here’s the truth: no system works if people are afraid to speak up.
Dr. Tejal Gandhi of the National Patient Safety Foundation says it plainly: ‘A nonpunitive approach to error reporting is the only way to learn.’
Too many hospitals punish nurses for scanning errors or doctors for prescribing mistakes. So they hide them. No one learns. No one improves.
Top-performing hospitals use the AHRQ Hospital Survey on Patient Safety Culture. They don’t just track errors-they track whether staff feel safe reporting them. The best score above the 75th percentile on ‘organizational learning’ and ‘teamwork across units.’
At one VA hospital, they started a ‘Safety Huddle’ before every shift. Anyone could say: ‘I’m worried about this med order.’ No names. No blame. Just discussion. Within a year, serious errors dropped by 55%.
It’s not about technology. It’s about trust.
What’s Changing in 2025
Medication safety isn’t standing still. The WHO extended its ‘Medication Without Harm’ initiative through 2027-with new focus on older adults on five or more drugs (polypharmacy) and safety in telehealth.
ISMP just released its 2024-2025 Best Practices, adding guidelines for AI-assisted prescribing. Early AI tools can now predict 89% of potential prescribing errors before they reach the patient-up from 67% with old CDS systems.
But here’s the warning: the FDA reported 214 adverse events tied to EHR usability in 2022-a 37% jump from 2021. AI won’t fix bad design. It might make it worse.
The real winners in 2025 will be the clinics and hospitals that combine smart tech with human-centered design. Not the ones with the fanciest software, but the ones that listen to nurses, pharmacists, and doctors-and build systems around their real workflows.
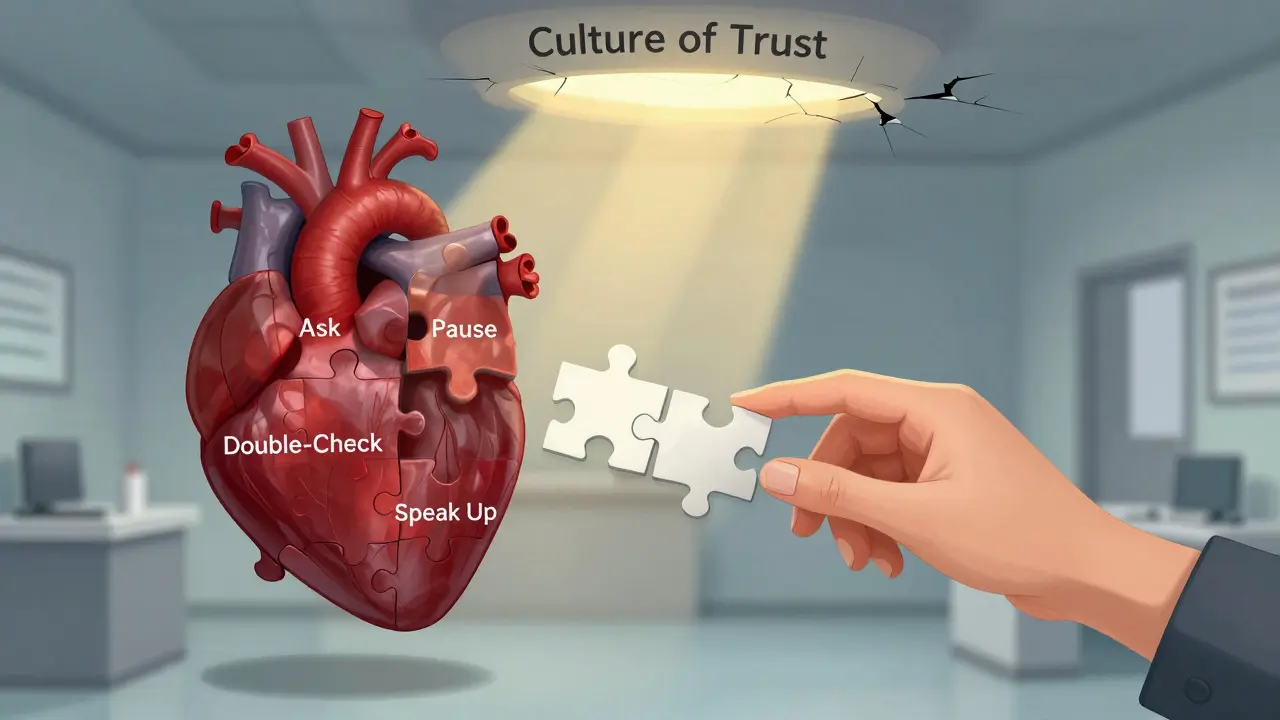
What You Can Do Today
You don’t need a $1 million system to make a difference.
- Ask before you give. ‘Why is this drug being given? What’s the goal?’ If you’re unsure, pause. Talk to the pharmacist.
- Use the five rights-every time. Even if you’re rushed. Even if you’ve done it a thousand times.
- Report near-misses. Not just errors. If you almost gave the wrong dose, say something. It saves lives.
- Push for better tech. If your EHR has 30 alerts per patient, ask: ‘Which ones are actually life-saving?’ Demand customization.
- Learn your high-alert meds. Know the ones that can kill with a typo. Memorize them. Talk about them with your team.
Medication safety isn’t a checklist. It’s a mindset. It’s saying: ‘I’m not just giving a pill. I’m holding someone’s life in my hands.’
What’s Next for Medication Safety
The future isn’t just AI or automation. It’s integration.
Imagine a system that knows your patient has kidney disease, takes six medications, lives alone, and missed their last refill. It flags the risk before the doctor even writes the script. That’s the goal.
But it won’t happen unless providers demand it. Until then, the best tool you have is your own judgment-and your willingness to speak up.
What are the most common causes of medication errors in hospitals?
The top causes are miscommunication between staff, poor handwriting on paper orders, incorrect dosing calculations, confusion between look-alike or sound-alike drug names (like hydralazine and hydroxyzine), and alert fatigue from overloaded electronic systems. Nurses and pharmacists report that rushed shifts and understaffing are the biggest contributing factors, not lack of knowledge.
How effective are barcode scanning systems at preventing errors?
Barcode-assisted medication administration (BCMA) reduces administration errors by about 41%, according to the Institute for Healthcare Improvement. However, effectiveness drops sharply if staff bypass the system-common during emergencies or when scanners malfunction. Full compliance requires strong leadership, user-friendly tech, and ongoing training.
Why do healthcare workers override so many drug interaction alerts?
Most alerts are false positives or irrelevant. A 2020 BMJ study found clinicians override 49-96% of alerts, especially when systems generate more than 20 per patient encounter. Many alerts warn about interactions with supplements patients stopped taking months ago, or low-risk combinations. When alerts don’t feel useful, staff stop paying attention-creating dangerous habituation.
What’s the difference between medication safety in hospitals versus primary care?
Hospitals have more resources: pharmacists on-site, electronic prescribing, barcode scanning, and formal error reporting systems. In primary care, only 32% of practices have structured medication reconciliation processes, compared to 89% in hospitals. Primary care providers often manage complex patients with no support, increasing the risk of errors from polypharmacy and poor communication with specialists.
Is medication safety training required by law?
No federal law mandates specific training hours, but The Joint Commission requires hospitals to demonstrate ongoing staff competency in medication safety as part of accreditation. Medicare penalizes hospitals with high error rates through payment reductions. Many states and institutions have internal policies requiring annual training, especially for high-alert medications.
What role do pharmacists play in medication safety?
Pharmacists are the last line of defense. The American Society of Health-System Pharmacists (ASHP) states they have the expertise to lead multidisciplinary efforts to prevent medication errors. In hospitals, pharmacists review every order, catch dosing mistakes, check for interactions, and educate staff. In clinics, they conduct medication reconciliations and help manage complex regimens. Their involvement cuts error rates by up to 80% in intensive care units.
Final Thought: Safety Isn’t a Program. It’s a Promise.
Medication safety isn’t something you implement. It’s something you live. Every time you pause before giving a drug. Every time you ask a colleague to double-check. Every time you report a near-miss without fear.
The tools are better than ever. The data is clear. What’s still missing is the courage to speak up-and the systems that let you do it without penalty.
If you’re a provider, your job isn’t just to treat. It’s to protect. And that starts with one simple question: ‘Am I sure this is right?’


Comments (10)
josue robert figueroa salazar
bcma is a joke. i bypass it every shift. no one cares until someone dies.
david jackson
I mean... think about it. We’re not just fighting human error here-we’re fighting a system designed by people who’ve never held a syringe in a 12-hour shift while three patients are coding and the printer’s out of labels. The alerts? They’re like a toddler screaming "FIRE!" every time you breathe too loud. And then we wonder why nobody listens anymore. It’s not that we’re lazy-it’s that we’ve been trained to ignore the noise. And now? The noise is the only thing left standing between us and disaster.
Jody Kennedy
Y’ALL. I just want to say-this post made me cry. Not because it’s sad. Because it’s TRUE. Last week, I caught a 10x overdose on insulin because I paused. Just paused. Asked the MD, "Why 50 units?" He said, "Oh, default." We fixed it. No blame. Just relief. We can do better. We HAVE to. Every. Single. Time.
christian ebongue
alert fatigue? more like alert autism. 23 warnings for a patient on 8 meds? yeah i clicked ignore. and i dont feel bad.
jesse chen
I’ve been in this game for 17 years… and I’ve seen the same mistakes repeat. Not because people are careless… but because the system doesn’t care. The barcode scanner doesn’t work in the OR. The EHR auto-fills the wrong dose. The nurse is alone at 3 a.m. with five patients. We need to stop blaming individuals and start redesigning the environment. It’s not about training more-it’s about listening more. And yes, I’ve reported near-misses. And yes, it changed something. Small, but real.
Joanne Smith
Let’s be real: the EHR vendors are selling snake oil wrapped in a 12-page compliance PDF. They don’t care if your nurse is overworked-they care if you pay for the premium module that adds 47 more alerts. I’ve seen a system that flags "possible interaction" between Tylenol and… water. I’m not kidding. And yet, they charge us $2 million a year for it. The real innovation? A pharmacist who shows up before the med goes in. Not a pop-up.
Prasanthi Kontemukkala
In my home country, we don’t have fancy scanners or AI. But we have something better: we talk. Before giving any high-alert med, we say the name out loud. We say the dose. We say the reason. And someone else listens. Not because it’s policy. Because we’ve seen what happens when we don’t. Simple. Human. Effective. Maybe we don’t need more tech. Maybe we just need to remember how to listen to each other.
Alex Ragen
Ah, yes-the existential quandary of pharmaceutical governance: when the epistemology of clinical decision-making is subsumed by algorithmic hegemony, the human agent becomes a mere interface between institutional failure and ontological vulnerability. We are not merely nurses or doctors-we are nodes in a broken cybernetic organism that mistakes compliance for care. And yet… we still sign the chart. With trembling hands.
Lori Anne Franklin
i just wanna say i love this post so much!! i used to think i was just bad at my job but now i realize its the system!! also i misspelled "medication" in my last report lol oops but i caught my own mistake before giving it!! yay!!
Bryan Woods
The data is unequivocal. Systemic interventions-such as pharmacist integration, simulation-based training, and reduction of non-actionable alerts-demonstrate statistically significant reductions in medication error rates. However, cultural resistance remains the most persistent barrier to adoption. Leadership must prioritize safety infrastructure over cost containment. The return on investment is measured in lives, not balance sheets.