Getting prescribed lithium for bipolar disorder doesn’t mean you can take any painkiller or diuretic without thinking twice. Even something as simple as ibuprofen for a headache or a water pill for high blood pressure can push your lithium levels into dangerous territory. And it doesn’t take much - just a few days of use, or even mild dehydration from a hot day or stomach bug, can trigger serious side effects. This isn’t theoretical. People have ended up in hospital - and some have died - because these interactions were overlooked.
Why Lithium Is So Sensitive
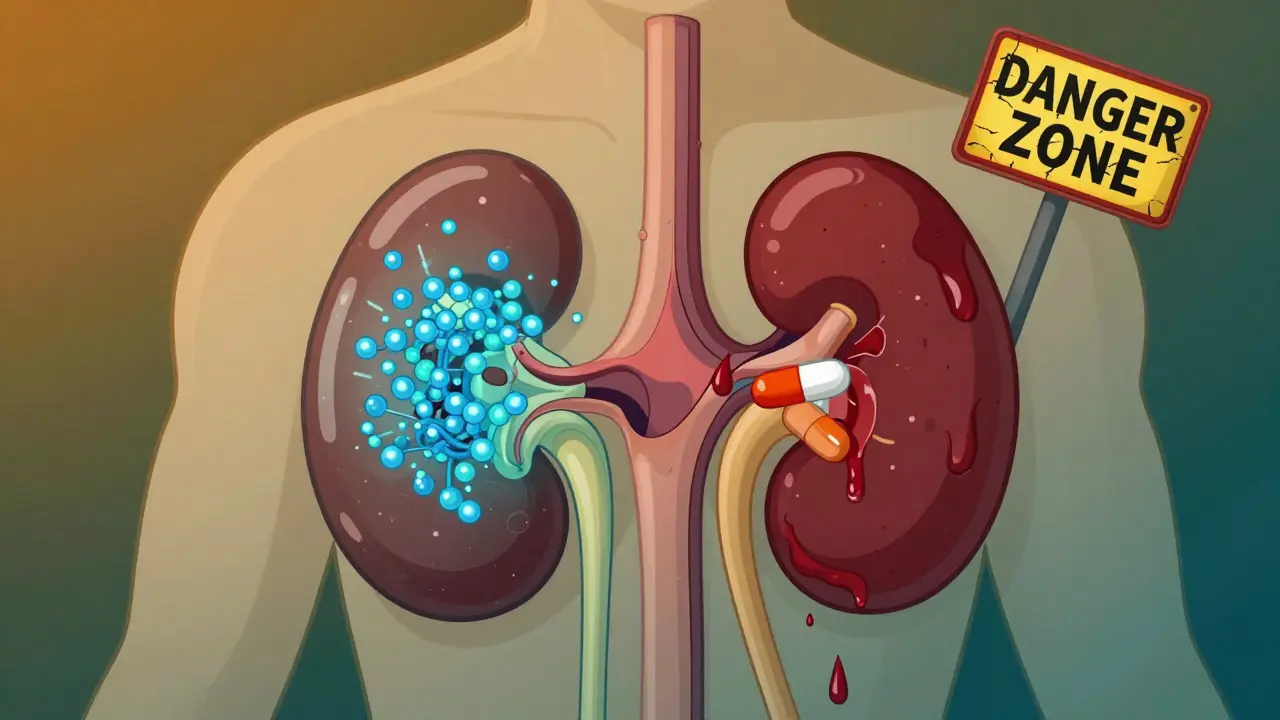
Lithium isn’t like most medications. It works in a very narrow window: between 0.6 and 1.2 mmol/L in your blood. Go below that, and it might not control your mood swings. Go above it, and you risk toxicity - which can mean shaky hands, confusion, vomiting, or even seizures. Your kidneys handle nearly all of it, filtering out about 95% unchanged. That means anything that messes with kidney function or fluid balance can cause lithium to build up fast.
That’s why age matters. If you’re over 65, your kidneys don’t filter as well. You’re already at 3.2 times higher risk of lithium toxicity, even without other drugs. Add in heart failure, diabetes, or kidney disease, and the danger multiplies. It’s not just about the pills you take - it’s about your whole body’s ability to clear lithium.
NSAIDs: The Silent Lithium Boosters
Non-steroidal anti-inflammatory drugs - think ibuprofen, naproxen, diclofenac, even celecoxib - are among the most common culprits. They reduce inflammation by blocking prostaglandins, which also helps your kidneys filter blood. When those prostaglandins drop, your kidneys slow down lithium clearance by 25% to 50%. In some cases, especially with indomethacin, the increase can hit 60%.
This doesn’t happen slowly. Lithium levels often spike within the first week of starting an NSAID. That’s why doctors warn against taking them regularly if you’re on lithium. Even occasional use - like popping a couple of pills for a bad back - can be risky if you’re not monitored. A case in New Zealand involved a 72-year-old woman who took ibuprofen for joint pain while already on lithium and an ACE inhibitor. Her lithium levels climbed unnoticed. She died from toxicity. Her levels had only been checked sporadically.
Not all NSAIDs are equal. Ibuprofen tends to raise lithium levels by 25-40%. Celecoxib is a bit gentler, around 15-30%. But no NSAID is truly safe. The safest approach? Avoid them entirely. If you need pain relief, talk to your doctor about alternatives like acetaminophen (paracetamol), which doesn’t interfere with lithium.
Diuretics: The Big Three
Diuretics - water pills - are another major red flag. They help with high blood pressure or swelling, but they also reduce the amount of fluid your body holds. Lithium rides along with that fluid. When fluid drops, lithium concentrates in your blood.
Thiazide diuretics like hydrochlorothiazide are the worst offenders. They can push lithium levels up by 25-50% in just 7-10 days. That’s why many doctors avoid prescribing them to people on lithium. Loop diuretics like furosemide (frusemide) are less risky, but still dangerous - they can raise levels by 10-25%. And potassium-sparing diuretics like spironolactone? Their effect is unpredictable. Some studies show a rise; others show no change. The uncertainty makes them risky too.
There’s one twist: not all diuretics raise lithium. Osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide actually lower lithium levels by 15-30%. That might sound helpful, but it’s not. It means your mood control could slip, and you’d need a dose adjustment. Either way, it’s a problem that needs medical oversight.
And don’t forget herbal diuretics. Many weight-loss teas and supplements claim to be “natural” and safe. But they work the same way as prescription diuretics - by flushing out fluid. If you’re taking these, your lithium levels could spike without you ever realizing it.

Dehydration: The Hidden Trigger
You don’t need to be on a drug to be at risk. Just getting dehydrated can do it. If you lose 2-3% of your body weight in water - say, from sweating in hot weather, vomiting, diarrhea, or even just forgetting to drink enough - lithium levels can jump 15-25%. That’s enough to cross into toxicity.
This is why travel is a big concern. Flying long-haul, especially in dry cabin air, can dehydrate you without you noticing. Traveling to hot climates? Even more dangerous. Gastroenteritis during a vacation? That’s a perfect storm: vomiting, diarrhea, less fluid intake, and lithium building up. People in these situations need to be warned - and monitored - before they even leave home.
Salt intake matters too. If you suddenly eat less salt - say, switching to a low-sodium diet - your body holds onto lithium. That can raise levels by 10-20%. On the flip side, eating more salt can help lower lithium levels. It’s not about going back to junk food, but about keeping your sodium intake steady. Sudden changes, whether up or down, can throw off your balance.
What to Do If You’re on Lithium
Here’s what actually works in real life, based on clinical guidelines from Australia, New Zealand, and the UK:
- Avoid NSAIDs if you can. Use paracetamol for pain instead. If you must take an NSAID, use the lowest dose for the shortest time possible.
- Never start a diuretic without talking to your psychiatrist or doctor. Thiazides are usually off-limits. If you need one, your lithium dose may need to be lowered, and your blood levels checked weekly for the first month.
- Drink water consistently. Don’t wait until you’re thirsty. Aim for 1.5-2 liters a day, more if you’re active, sick, or in heat. Avoid alcohol and caffeine - they dehydrate you.
- Don’t change your salt intake suddenly. Eat about the same amount of salt every day. Don’t go low-sodium unless your doctor says so.
- Get blood tests done regularly. Even if you feel fine, lithium levels should be checked every 3-6 months. After starting a new drug or if you get sick, get tested within a week.
- Know the early warning signs. Diarrhea, dizziness, drowsiness, shaky hands, or nausea? These are often the first signs of lithium toxicity. Don’t wait. Call your doctor or go to the emergency room.
Some people think, “I’ve been on lithium for years, I know my body.” But lithium doesn’t care how long you’ve been on it. Your kidneys change. Your diet changes. You get older. That’s why monitoring doesn’t stop.

When to Seek Help Immediately
Don’t wait for symptoms to get worse. If you’re on lithium and experience any of these, get medical help right away:
- Severe diarrhea or vomiting
- Confusion, memory problems, or trouble speaking
- Uncontrollable shaking or muscle twitching
- Blurred vision or ringing in your ears
- Seizures or loss of consciousness
These aren’t side effects - they’re signs of lithium poisoning. Left untreated, it can cause permanent kidney damage or death. Emergency treatment involves stopping lithium, IV fluids, and sometimes dialysis.
The Bottom Line
Lithium is a powerful tool for managing bipolar disorder - but it’s not a drug you can treat casually. NSAIDs, diuretics, and dehydration aren’t just minor risks. They’re red flags that can turn a stable treatment into a medical emergency. The good news? These risks are well-known, predictable, and avoidable. You don’t need to stop living - you just need to be smart.
Keep your doctor informed about every medication, supplement, or change in your routine. Stay hydrated. Don’t guess with salt. Get your blood tested. And if something feels off - don’t brush it off. Lithium toxicity doesn’t always come with a warning. But you can stop it before it starts.
Can I take ibuprofen while on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 25-40% within days, increasing your risk of toxicity. If you need pain relief, paracetamol (acetaminophen) is safer. If you must take ibuprofen, do so only for a short time and get your lithium levels checked within a week.
What diuretics are safe with lithium?
No diuretic is completely safe. Thiazides like hydrochlorothiazide are the most dangerous, often raising lithium levels by over 50%. Loop diuretics like furosemide carry a lower but still significant risk. Potassium-sparing diuretics have unpredictable effects. Always consult your doctor before starting any diuretic - lithium may need to be reduced and monitored closely.
How does dehydration affect lithium levels?
Dehydration causes your blood volume to drop, which concentrates lithium in your bloodstream. Losing just 2-3% of your body weight in water can raise lithium levels by 15-25%. This can happen from heat, illness, exercise, or even flying. Drink water consistently - don’t wait until you’re thirsty.
Can I drink alcohol while on lithium?
Alcohol dehydrates you and can worsen lithium side effects like dizziness and drowsiness. It also affects your liver and kidneys, which can interfere with lithium clearance. It’s best to avoid alcohol or limit it to very small amounts - and never drink heavily.
How often should lithium levels be checked?
If you’re stable, every 3-6 months is standard. But if you start a new medication - especially an NSAID or diuretic - get tested within 5-7 days and again at 2 weeks. After illness, travel, or dehydration, check your levels too. Regular monitoring saves lives.
What are the first signs of lithium toxicity?
Early signs include diarrhea, nausea, dizziness, drowsiness, shaky hands, and mild confusion. These often appear before more serious symptoms like blurred vision, ringing in the ears, or seizures. Don’t ignore them - call your doctor immediately if you notice these, especially if you’ve recently started a new drug or been sick.
Can lithium toxicity cause permanent damage?
Yes. Severe or repeated episodes of lithium toxicity can cause permanent kidney damage, especially in older adults or those with pre-existing kidney issues. Even if you recover, your kidney function may not return to normal. That’s why prevention - through monitoring and avoiding interactions - is critical.
Should I stop lithium if I need surgery?
Never stop lithium on your own. Your doctor may advise holding it temporarily before surgery, especially if you’ll be fasting or receiving IV fluids. But stopping it abruptly can trigger a relapse. Always discuss this with your psychiatrist and surgeon ahead of time - they’ll coordinate a safe plan.
Next Steps for Patients
If you’re on lithium, start by reviewing your current medications with your doctor. Make a list of everything you take - even over-the-counter painkillers, herbal teas, or supplements. Ask: “Could this affect my lithium?” Then, set up a hydration and salt intake routine. Drink water daily. Keep your salt intake steady. Get your blood tested on schedule. And if you’re planning to travel, get advice before you go.
Lithium keeps many people stable. But it demands respect. The risks are real - but they’re manageable. You don’t have to live in fear. Just stay informed, stay connected to your care team, and don’t ignore the small things. They’re the ones that matter most.

Comments (8)
Darryl Perry
Lithium toxicity isn't some rare edge case-it's a predictable disaster waiting to happen. If your doctor didn't explicitly warn you about NSAIDs and dehydration, they're not doing their job. No excuses. Get tested. Stop taking ibuprofen like it's aspirin. Your kidneys aren't magic.
Windie Wilson
So let me get this straight-I can’t take Advil for my period cramps, can’t drink coffee, can’t fly to see my mom, and now I’m supposed to weigh my salt like a lab rat? Thanks, medicine. I’ll just sit here in a dark room humming bipolar lullabies.
Daniel Pate
The pharmacokinetics here are fascinating. Lithium’s renal clearance is exquisitely sensitive to prostaglandin inhibition-NSAIDs blunt the afferent arteriole dilation, reducing GFR and tubular flow. But the real issue isn’t the mechanism-it’s the systemic failure of patient education. Why are we relying on patients to remember obscure drug interactions when the system should auto-flag these combinations? The burden shouldn’t be on the person managing a chronic mental illness to be a pharmacologist.
And dehydration? A 2% fluid loss triggering toxicity? That’s not a side effect-it’s a design flaw in how we monitor chronic meds. We don’t do this with warfarin or digoxin. Why lithium?
Cecelia Alta
Okay but have you met the average person on lithium? I’ve seen people take a handful of ibuprofen because their back hurt, then go on vacation to Florida, drink three margaritas, forget to drink water, and then show up at the ER with tremors and vomiting like it’s a plot twist in a medical drama. And then they’re mad the system didn’t protect them. Honey. You’re on a drug that can kill you if you sneeze wrong. The warning signs are written in neon. You just chose to squint.
And don’t even get me started on those ‘natural’ diuretic teas. You think your ‘detox’ tea is any safer than hydrochlorothiazide? It’s literally the same chemistry with a yoga logo. You’re not healing your soul-you’re poisoning your kidneys. And yes, I’ve seen it. Multiple times. In my own family.
Stop acting like this is a mystery. It’s not. It’s negligence dressed up as ‘I didn’t know.’ You knew. You just didn’t care enough to ask.
And before you say ‘but my doctor never told me’-your doctor told you 17 times. You just tuned out because you were tired of being told what you can’t do. That’s not the system’s fault. That’s you.
And yes, I’m that person who yells at strangers in the pharmacy when they grab the Advil next to the lithium bottle. I’ve seen too many people die because someone thought ‘it’s just one pill.’
steve ker
Lithium is for weak people who cant handle life without chemicals. NSAIDs? Dehydration? Grow up. Stop being so fragile. Just take your pills and stop complaining. Doctors are lazy anyway.
gary ysturiz
Just wanted to say-this post saved my life. I was about to start ibuprofen for my knee pain. I’d been on lithium for 8 years and never thought twice. But after reading this, I called my psychiatrist. We switched me to acetaminophen and set up monthly blood tests. I feel better than I have in years. You’re not alone. And you’re not weak for needing help. You’re brave for staying on top of it.
Bryan Wolfe
YES. YES. YES. This is the kind of info that needs to be screamed from the rooftops!! I’ve been on lithium for 12 years, and I finally got my bloodwork done after my doctor said ‘you’re fine’-turns out my levels were creeping up because I started taking melatonin for sleep (which has mild diuretic effects). I didn’t even know!!
So now I have a hydration tracker on my phone. I drink water before coffee. I keep a salt shaker on the table. I text my psychiatrist every time I get sick. I tell every new friend I meet: ‘If I seem off, don’t assume I’m being dramatic-check if I’ve been drinking water.’
You’re not being paranoid-you’re being smart. And if you’re reading this and you’re on lithium? You’re doing great. Keep going. You’ve got this. And if you’re a caregiver? Thank you. You’re the unsung hero in this story.
And to the person who said ‘just stop taking it’? You don’t get it. Lithium isn’t a choice-it’s a lifeline. Don’t shame the people who are fighting to stay alive. Support them. Share this. Save someone.
Rinky Tandon
From a clinical pharmacology standpoint, the nephrotoxic synergy between lithium and thiazide diuretics is well-documented in the NICE guidelines and the Australian Medicines Handbook-both classify this as a Category A interaction with high clinical significance. The mechanism involves downregulation of sodium-chloride cotransporters in the distal convoluted tubule, which increases lithium reabsorption via the sodium-lithium countertransport system. This is not anecdotal-it’s evidence-based. Yet, primary care providers continue to prescribe hydrochlorothiazide to patients on lithium without consulting psychiatric pharmacists. This is systemic failure.
Additionally, the pharmacokinetic variability in elderly populations-particularly those with reduced creatinine clearance-is grossly underappreciated. A 2021 meta-analysis in the Journal of Clinical Psychopharmacology showed that patients over 65 with eGFR <60 mL/min had a 4.7-fold increased risk of toxicity following NSAID exposure. Yet, no automated EHR alerts exist for this in 87% of U.S. clinics.
Until we implement mandatory electronic decision support for lithium-drug interactions, we are not practicing medicine-we are gambling with human lives. And yes, this includes herbal diuretics. The FDA doesn’t regulate them because they’re ‘natural,’ but their pharmacodynamic effects are identical to pharmaceuticals. This is regulatory negligence.
Stop normalizing this risk. This isn’t about ‘being careful.’ It’s about systemic accountability.