Switching from a brand-name drug to a generic version is supposed to be safe, simple, and cost-effective. Most of the time, it is. But for some people, a seemingly minor change in the pill they take can trigger a chain reaction of strange symptoms-headaches that won’t quit, swelling in the ankles, heart palpitations, or skin rashes that appear out of nowhere. These aren’t just "all in your head." They’re real, documented side effects tied to differences in generic medications that most people never see coming.
Why a Generic Might Not Feel Like the Same Drug
The FDA says generics must contain the same active ingredient, dose, and route of delivery as the brand-name version. That’s true. But what they don’t tell you is that the rest of the pill-what’s holding the active ingredient together-can be completely different. These are called excipients: fillers, dyes, binders, flavorings, and preservatives. And while they don’t treat your condition, they can definitely mess with your body. Take levothyroxine, the thyroid medication. Brand-name Synthroid and its generics all have the same active ingredient: levothyroxine sodium. But one generic might use cornstarch as a filler, another uses lactose. If you’re lactose intolerant, that tiny difference can cause bloating, diarrhea, or even throw your thyroid levels off. A 2023 GoodRx analysis found that 23.7% of patients switching to generic thyroid meds reported new side effects. That’s more than one in five people. The same thing happens with antidepressants, blood pressure pills, and epilepsy drugs. A patient on brand-name Adderall might feel fine, but switch to a generic version made by a different company, and suddenly they’re getting daily headaches and stomach cramps. Why? Because the generic might use a different coating or a new dye-like Red 40 or Yellow 5-that triggers reactions in sensitive people. These aren’t rare. The FDA’s adverse event database recorded over 1,800 reports between 2020 and 2023 where patients directly linked new symptoms to a generic switch.High-Risk Medications: Where Small Changes Cause Big Problems
Not all generics are created equal. Some drugs have what’s called a narrow therapeutic index (NTI). That means the difference between a dose that works and one that’s dangerous is tiny. Even a 5% variation in how the drug is absorbed can lead to serious consequences. The FDA lists 18 NTI drugs. The most common ones you’ll hear about are:- Warfarin (Coumadin) - a blood thinner. Switching generics can increase bleeding risk. One study found 14.7% of patients had unexpected bleeding after switching manufacturers.
- Levothyroxine (Synthroid) - thyroid hormone. Small changes in absorption can cause fatigue, weight gain, or heart palpitations.
- Phenytoin (Dilantin) - an anti-seizure drug. A slight drop in blood levels can trigger seizures.
- Liium - used for bipolar disorder. Changes in levels can lead to mood crashes or mania.

What the Manufacturer Doesn’t Tell You
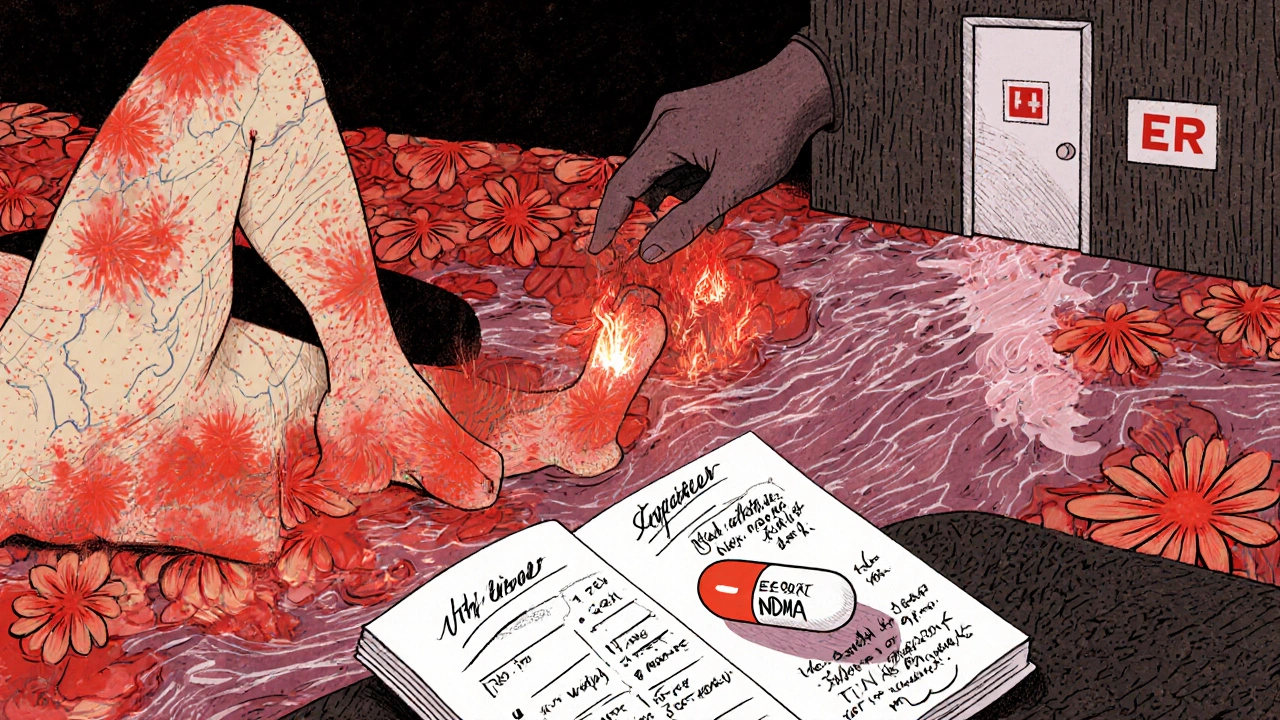
Most people don’t realize that the same generic drug can come from different factories, sometimes even different countries. Over 70% of the active ingredients in U.S. generics are made overseas-in India and China. And while the FDA requires good manufacturing practices, inspections aren’t always consistent. A 2022 government report found that nearly 1 in 5 foreign generic factories had delays or access issues during inspections. Then there’s the recall issue. In 2018 and 2019, a contamination in valsartan (a blood pressure drug) led to a massive recall affecting over 2 million people. The culprit? A cancer-causing chemical called NDMA. It wasn’t in the brand-name version. It was introduced during the manufacturing process of a specific generic batch. That’s why lot numbers matter. If you notice new side effects after a refill, check the pill’s imprint code and the manufacturer name on the bottle. Write it down. If you switch back to the same generic and the symptoms return, you’ve found your trigger.Red Flags: When to Call Your Doctor Right Away
Not every new symptom means you need to panic. But some reactions are serious-and they need immediate attention. Call your doctor within 24 hours if you experience:- Severe stomach pain, vomiting, or diarrhea lasting more than 48 hours
- New or worsening dizziness, confusion, or tremors
- Swelling in your legs, ankles, or face that didn’t happen before
- A sudden, unexplained rash or hives
- Heart rate that’s consistently over 100 or below 50 beats per minute
- Stevens-Johnson Syndrome: A painful, blistering rash that spreads, often starting on the face or chest, with sores in your mouth, eyes, or genitals. Linked to lamotrigine, allopurinol, and some antibiotics.
- Priapism: A painful erection lasting more than 4 hours. Seen with trazodone and bupropion.
- Signs of an allergic reaction: Trouble breathing, swelling of the throat, rapid pulse.
What You Can Do to Protect Yourself
You don’t have to avoid generics. They’re safe for most people and save billions in healthcare costs. But you need to be smart about it. Here’s what works:- Ask your pharmacist: "Which manufacturer made this batch?" Write it down.
- Keep a simple log: Date, medication, manufacturer, any new symptoms.
- If you feel worse after a refill, don’t assume it’s "just stress." Go back to your doctor and say: "I switched generics and now I’m having X symptom."
- For high-risk drugs (thyroid, blood thinners, epilepsy meds), ask if you can stay on the same generic manufacturer. Many doctors will write "Dispense as written" or "Do not substitute" on the prescription.
- Report side effects to the FDA through MedWatch. Even one report helps track patterns.
The Bigger Picture: Why This Isn’t Going Away
The push for generics is driven by money. The U.S. spends over $227 billion a year on generic drugs. Medicare saved $1.67 trillion from 2006 to 2022 thanks to them. That’s huge. But savings shouldn’t come at the cost of patient safety. New legislation is being considered. The Generic Drug Safety Act, introduced in early 2024, would require manufacturers to notify doctors and pharmacists whenever they change excipients. That’s a step forward. For now, the system still treats all generics as interchangeable. But your body doesn’t care about FDA approval forms. It reacts to what’s in the pill-and what’s not. If you’ve ever thought, "This doesn’t feel right," and then found out you switched generics? You weren’t imagining it. You were right to listen.Can generic medications cause different side effects than brand-name drugs?
Yes. While generics must contain the same active ingredient as the brand-name version, they can differ in inactive ingredients like fillers, dyes, and preservatives. These excipients can trigger reactions in sensitive individuals-such as digestive issues, headaches, skin rashes, or even changes in drug absorption. For drugs with a narrow therapeutic index (like warfarin or levothyroxine), even small differences can lead to serious side effects.
Which generic drugs are most likely to cause unexpected side effects?
Drugs with a narrow therapeutic index are highest risk. These include levothyroxine (for thyroid), warfarin (blood thinner), phenytoin (anti-seizure), lithium (mood stabilizer), and some antidepressants like lamotrigine. Studies show higher rates of side effects after switching generics in these categories-up to 24% for thyroid meds and 15% for blood thinners. Also watch for generics of epilepsy drugs, psychiatric medications, and certain blood pressure pills.
What should I do if I think my generic medication is causing side effects?
Don’t stop taking the medication on your own. Contact your doctor or pharmacist immediately. Note the exact name of the manufacturer on your prescription bottle and describe your symptoms clearly. If symptoms started within 1-2 weeks of switching, it’s likely related. Your provider may switch you back to the brand or to a different generic. Keep a log of what you took and when symptoms appeared-it helps identify patterns.
How can I avoid side effects when switching to a generic?
Ask your pharmacist which manufacturer made your generic and write it down. If you’ve had a good experience with one brand, ask your doctor to specify "Dispense as written" or "Do not substitute" on your prescription. For high-risk drugs, stick with the same manufacturer every refill. Keep a simple journal: date, drug name, manufacturer, symptoms. Report any new issues to your doctor and consider filing a report with the FDA’s MedWatch program.
Are generic medications less safe than brand-name drugs?
No-most generics are just as safe and effective. The FDA requires them to meet strict standards for bioequivalence. But safety doesn’t mean identical for everyone. Variations in excipients, manufacturing quality, and individual sensitivity mean some people will react differently. The risk is low overall, but it’s real enough that patients and doctors should be aware, especially with high-risk medications. The goal isn’t to avoid generics-it’s to use them wisely.


Comments (13)
Jennifer Shannon
Wow, this post really hit home for me. I switched from Synthroid to a generic last year and suddenly I was exhausted all the time, my hair started falling out, and I gained ten pounds without changing anything else. My doctor said it was "just stress" until I brought up the switch. Then she looked at the bottle and said, "Oh. That’s a different manufacturer." We switched back and within two weeks, I felt like myself again. I didn’t realize how much those little fillers could mess with your body. It’s wild that the FDA doesn’t require them to label which excipients are used. We’re basically guinea pigs.
Suzan Wanjiru
As a pharmacist I see this every week. Patients come in saying "I don’t feel right" and nine times out of ten it’s because their generic was switched without them knowing. We don’t get told when the manufacturer changes. We just dispense what the insurance pushes. I’ve started asking patients: "Which brand did you take last time?" and writing it down. It’s extra work but it saves lives. Especially with warfarin. One patient had a bleed because the new generic absorbed slower. He almost died. Don’t assume all generics are equal. Ask for the manufacturer name every time.
Bryson Carroll
Look I get it people are scared of generics but come on. This is just fearmongering wrapped in a lab coat. The FDA approves these things. If they weren’t safe they wouldn’t be on the market. You’re telling me that a pill with the same active ingredient can somehow be dangerous because it has cornstarch instead of lactose? What next, are we going to ban aspirin because some brands use talc? This isn’t science. It’s placebo effect dressed up as a medical mystery. Stop blaming the pill and start blaming your anxiety.
Manjistha Roy
I’ve been on levothyroxine for 12 years and I’ve switched generics six times. Four of those times I had weird symptoms-brain fog, tremors, heart racing. I started tracking the manufacturer on the bottle. I found out that the one with the white oval pill with ‘93’ on it always made me feel awful. The one with the blue capsule with ‘23’ on it? Perfect. Now I only accept that one. My doctor doesn’t even question it anymore. I keep a printed list in my wallet. If you’re on a high-risk med, do this. It’s not paranoia. It’s power.
Henrik Stacke
As someone who has lived in both the US and the UK, I find this discussion fascinating. In the UK, we have a similar system, but pharmacists are legally required to inform patients when a generic substitution occurs. Here in the US, it’s a silent switch. No warning. No consent. And yet, patients are expected to be medical detectives. This isn’t just about excipients-it’s about transparency. The pharmaceutical industry profits from this opacity. And we, the patients, pay the price-in health, in stress, in trust. Something needs to change.
Katy Bell
I had a rash after switching to a generic antidepressant. Didn’t think much of it. Then I got a new refill and the pill looked different. I looked up the manufacturer and saw a recall notice for that batch. Turns out, the dye was contaminated. I called my doctor and we switched back to the brand. I was so scared. I didn’t know what to believe. Now I always check the pill imprint and the lot number. I even took a photo of the bottle every time. It sounds obsessive but it saved me. Please, if you feel off after a refill-don’t ignore it. It’s not in your head.
Jennifer Skolney
Just wanted to say thank you for this post. I’ve been silent about this for years because I thought I was being dramatic. I switched from Lamictal to a generic and got Stevens-Johnson Syndrome. I was in the hospital for three weeks. My skin peeled off. I thought I was dying. No one believed me until I showed them the bottle. The generic had a different dye. Now I only take the brand. My insurance hates me. But I’m alive. And I’m not letting them take that from me again.
Olanrewaju Jeph
As a nurse in Lagos, I’ve seen patients in Nigeria struggle with counterfeit generics. But even in the U.S., where regulation is stronger, the problem persists. The real issue isn’t the active ingredient-it’s the lack of traceability. In Nigeria, we know the batch number and source. In the U.S., we don’t. Patients are left guessing. This isn’t about being anti-generic. It’s about accountability. Manufacturers should be required to provide batch-specific excipient lists online. Patients deserve that right. Not just for safety, but for dignity.
Pramod Kumar
Let me tell you about the time I switched generics and my brain felt like it was wrapped in wet cotton. I couldn’t focus. I forgot names. I zoned out during meetings. I thought I was getting dementia. Then I noticed the pill was a different color. I looked up the manufacturer. It was the same one that had the recall for the valsartan contamination. I called my pharmacist. They didn’t know. I called my doctor. They didn’t care. I went to the ER. They took one look at my pill bottle and said, "Oh. That’s the one." I didn’t know I had to become a detective just to stay alive. Now I carry a laminated card in my wallet with my medication, manufacturer, and symptoms. I’m not crazy. The system is broken.
Ragini Sharma
so like… i switched generics and got a rash. then i switched back and it went away. then i switched again and it came back. so i’m like… ok this is weird. so i looked at the bottle and the pill had a different number on it. so i googled it and found a reddit thread from 2021 where 200 people had the same problem with that exact pill. i printed it out and took it to my dr. she was like ‘huh. i didn’t know that.’ i’m just a person. not a scientist. but i figured it out. why should i have to?
Linda Rosie
Thank you for sharing this. I’ve been advocating for this issue for years. The FDA’s bioequivalence standards are insufficient for NTI drugs. We need a tiered system: high-risk generics should be labeled with manufacturer and excipient details. Patients deserve informed choice. This isn’t about fear. It’s about informed consent.
Vivian C Martinez
I’m a nurse and I’ve seen too many patients suffer silently because they don’t know how to speak up. If you feel different after a refill, say something. Write down the manufacturer. Bring the bottle. Don’t wait until you’re in the ER. Your voice matters. And if your doctor brushes you off? Find another one. You deserve care that listens.
JD Mette
I’ve been on warfarin for 15 years. I switched generics once. My INR spiked. I almost bled out. I didn’t know what happened until I checked the bottle. Now I only take the same one. I’ve had to fight my insurance every time. They keep trying to switch me. I keep fighting back. I’ve saved my own life by being stubborn. You’re not being difficult. You’re being smart.