When a brand-name drug loses its patent, you’d expect prices to drop fast. That’s usually how it works - generic competitors step in, and everyone wins with lower costs. But sometimes, the brand company itself releases a version of the drug under a generic label. That’s an authorized generic. It’s not a knockoff. It’s the exact same pill, same factory, same packaging - just without the brand name. And in the next five years, these products are going to play a bigger, more complicated role in how drugs are priced and distributed in the U.S.
What Exactly Is an Authorized Generic?
An authorized generic isn’t approved through the usual generic drug process (the ANDA). Instead, it’s made by the original brand manufacturer and sold under a generic name, often to pharmacies or distributors who then sell it as a cheaper alternative. The FDA has tracked these since 1999, and between 2010 and 2019, there were 854 launches. Most of them came after the first traditional generic entered the market - not before. Why? Because brand companies didn’t want to hurt their own sales. They waited until generics started cutting into profits, then dropped their own version to compete directly. These aren’t rare. They’re common in oral tablets and capsules - the easiest drugs to copy. Think blood pressure meds, cholesterol pills, or antidepressants. For drugs that once sold for $100 a month, an authorized generic might sell for $20. But here’s the catch: the same company that made the $100 version is now selling the $20 one. That means they’re still in control of the market, even after losing patent protection.Why Companies Use Authorized Generics
It’s not charity. It’s strategy. When a brand drug’s patent expires, the first generic company to file gets 180 days of exclusivity. That’s a big deal. They can be the only low-price option for half a year. But if the brand company launches an authorized generic during that window, they split the market. The first generic can’t dominate. Prices stay lower, but the brand company still gets a slice of the revenue. In markets where 180-day exclusivity applied, about 70% of authorized generics launched before or during that period. That’s not accidental. It’s calculated. The brand company doesn’t want to lose control. They don’t want a single generic to become the default choice. By entering with their own version, they keep pricing pressure on the market - and on themselves. It’s also a way to avoid being completely pushed out. Without an authorized generic, a brand drug’s sales can drop 80% or more in the first year after patent loss. With one, the drop might be 50%. That’s still a big hit - but not a collapse.The Shift: Delayed Launches Are Becoming Rare
A few years ago, brand companies would wait months - even years - to launch an authorized generic. They’d let the first generic take the market, then swoop in later to undercut them. That practice is fading. According to RAPS in June 2025, the number of delayed launches has dropped significantly. Why? Two reasons. First, regulators and lawmakers are watching. There’s growing pressure to make sure generics reach the market quickly. Delaying an authorized generic to protect brand revenue looks like anti-competitive behavior. The FDA, Congress, and even private insurers are asking tough questions. Second, the market is changing. With more drugs losing patents - over $200 billion in annual sales between 2025 and 2030 - companies can’t afford to sit back. They need to move fast. If they wait too long, a competitor might lock in market share. Launching an authorized generic early keeps them relevant. This shift is good for patients. Faster access to low-cost versions means lower out-of-pocket costs. But it’s also forcing brand companies to rethink their entire post-patent strategy.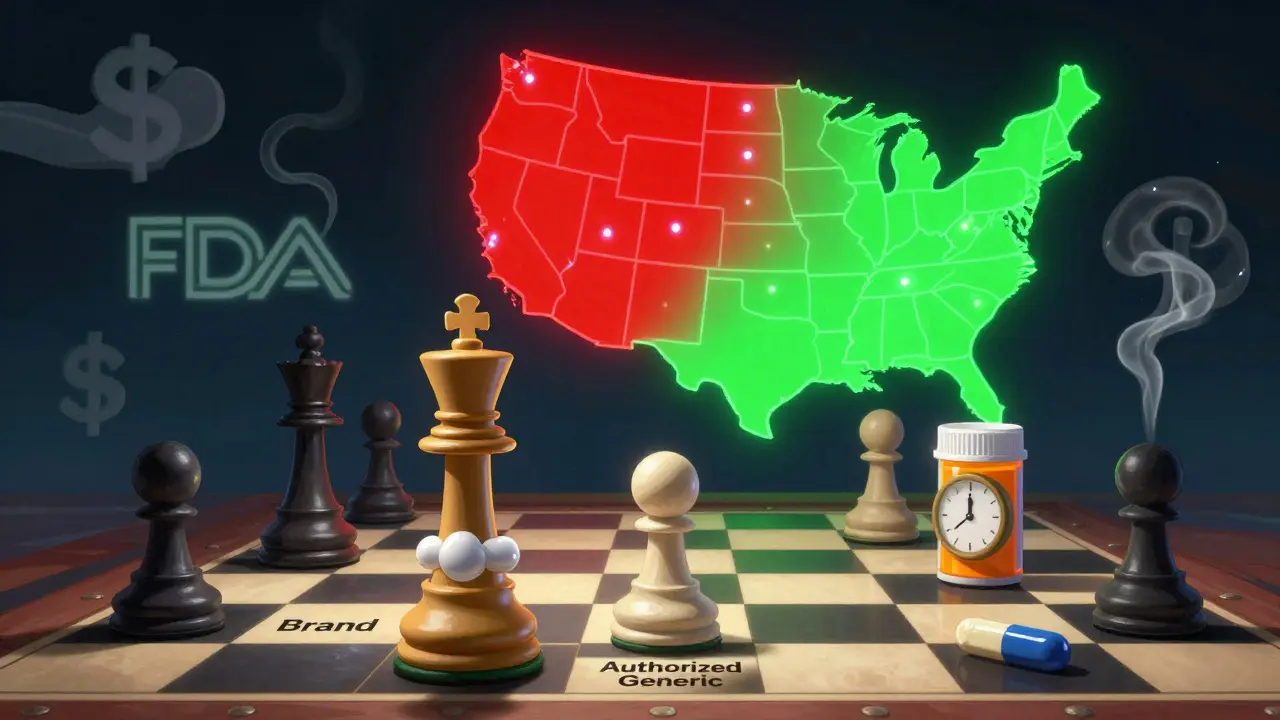
The FDA’s New Pilot Program Changes Everything
In October 2025, the FDA announced a new pilot program: faster ANDA reviews for generic drugs made and tested entirely in the U.S. This isn’t just about speed. It’s about supply chain control. After years of relying on overseas manufacturing - especially from India and China - the U.S. government is pushing for domestic production. For authorized generics, this matters a lot. If a brand company wants to make an authorized generic, they now have a strong incentive to produce it in the U.S. Faster approval means they can get to market quicker. And if they’re already making the branded version in the U.S., switching to an authorized generic version is easy. No new factory. No new supply chain. Just a new label. This could lead to more authorized generics made in America. It could also make it harder for foreign manufacturers to compete. Traditional generics from overseas might face longer approval times. That gives U.S.-based brand companies a structural advantage - even in the generic space.What’s Next for the Market?
The U.S. generic drug market is growing. It hit $138 billion in 2024 and is expected to reach nearly $200 billion by 2034. That growth is driven by blockbuster drugs losing patent protection. Ustekinumab, vedolizumab, and others - drugs that made billions for their makers - are now open to competition. The opportunity for biosimilars alone could hit $25 billion by 2029 in oncology and immunology. Authorized generics will be part of that wave. But they won’t dominate. They’ll coexist with traditional generics, biosimilars, and even new pricing models like value-based contracts. What’s changing is their role. They’re no longer just a weapon against competitors. They’re becoming a tool for managing market transitions. Companies are starting to see them as a bridge - not a barrier. Launching an authorized generic early helps stabilize prices. It prevents wild swings in drug costs. It gives pharmacies and insurers predictable pricing. That’s valuable in a system that’s under pressure to control spending.
The Bigger Picture: Savings, Costs, and Policy
Generic drugs saved the U.S. healthcare system $467 billion in 2024. That’s over $3.4 trillion in the last decade. Authorized generics contributed to that. But they also added complexity. When a brand company sells its own generic, it’s harder to measure true price competition. Are prices falling because of real competition - or because the brand is just playing both sides? A 2025 JAMA Health Forum study found that when brand companies extended market exclusivity - even by a few months - it cost commercial insurers and Medicare over $5 billion in extra spending. Authorized generics, when used to delay true competition, made that worse. But when used transparently and early, they helped keep prices down. Policy is catching up. Regulators are looking at transparency. They want to know who’s making what, where, and when. The FDA’s listing system is still manual. It’s slow. That’s changing. More real-time data is coming. And with it, more accountability.What This Means for Patients and Providers
For patients, the future looks better. More authorized generics mean more low-cost options. More domestic production means fewer supply shortages. More transparency means fewer surprises. For prescribers, it means more choices - but also more confusion. Is the generic you’re prescribing made by the brand company? Is it the same as the one from a third-party maker? Pharmacists will need better tools to explain the difference. For pharmacies, it’s a chance to negotiate better prices. If there are two versions of the same drug - one from the brand, one from a third party - they can play them against each other. That’s good for their margins and for patient access.The Bottom Line
Authorized generics aren’t going away. They’re evolving. The days of using them to block competition are ending. The future belongs to those who use them to speed up access, stabilize prices, and support domestic manufacturing. The next five years will be defined by one question: Will authorized generics be a tool for fairness - or a loophole for profit? Right now, the signs point to fairness. But only if regulators keep pushing, and if companies keep adapting.Are authorized generics the same as regular generics?
Yes, in every way that matters. Authorized generics are made by the original brand manufacturer using the same formula, same ingredients, and same factory as the branded drug. The only difference is the label. They’re not copies - they’re the real thing sold under a generic name. Regular generics are made by other companies after reverse-engineering the drug. Both are FDA-approved and equally safe.
Why do brand companies make authorized generics?
To stay in the game after patent expiration. Instead of losing all revenue when generics enter, they keep a piece of the market by offering their own low-cost version. It helps them avoid a total sales collapse and gives them control over pricing. It also lets them compete directly with other generics, especially during the first generic’s 180-day exclusivity period.
Do authorized generics lower drug prices?
Usually, yes - but not always. When an authorized generic enters the market early, it puts pressure on other generics to lower prices too. That drives down costs for patients and insurers. But if a brand company delays launching one to protect their own sales, prices stay high. The trend now is toward earlier launches, which is good for affordability.
Is the FDA doing anything to change how authorized generics work?
Yes. In October 2025, the FDA launched a pilot program that fast-tracks approval for generic drugs made and tested entirely in the U.S. This gives brand companies an incentive to produce authorized generics domestically. It also makes it harder for foreign manufacturers to compete. This policy shift is reshaping the entire generic drug landscape.
Will authorized generics disappear as biosimilars grow?
No. Biosimilars are for complex biologic drugs - like those used for cancer or autoimmune diseases. Authorized generics are for simpler, small-molecule pills. They serve different markets. In fact, as biologics lose patents, we’ll see more authorized generics for older, high-volume drugs like statins and antihypertensives. Both will coexist.
How can I tell if my prescription is an authorized generic?
Check the label. Authorized generics often list the brand manufacturer’s name under the generic name. For example, you might see "Simvastatin (made by Merck)" instead of just "Simvastatin." Your pharmacist can also tell you. Some insurance plans even list them separately in their formularies. If you’re unsure, ask.


Comments (14)
Jeane Hendrix
So authorized generics are basically the brand company saying 'hey we still got this' after the patent expires? Kinda wild they can do that. I get why they do it, but it still feels like a loophole. At least prices are dropping, right?
Rachel Wermager
Let’s be real-this isn’t innovation, it’s regulatory arbitrage. The FDA’s ANDA pathway was designed for independent generics to foster competition. When the originator manufactures the ‘generic,’ they’re gaming the system by preserving margin while appearing to comply. The 180-day exclusivity carve-out is the real villain here, and authorized generics are the brand’s scalpel to dissect it.
Leonard Shit
lol so the company that charged you $100 for a pill now sells you the exact same pill for $20… and we’re supposed to cheer? 🤡
At least they’re not outright blocking generics anymore. Progress? Maybe. Still feels like watching a fox guard the henhouse.
Brian Anaz
Why are we letting foreign companies make our meds? If the brand makes the generic in the U.S., that’s good for jobs. If India or China makes it, we’re just importing trouble. FDA’s new pilot? Long overdue. Buy American. End of story.
Molly McLane
As someone who works in pharmacy, this shift is actually helping. Patients are less confused when they see the same manufacturer on the generic label. We used to get calls every day asking if ‘this generic is legit.’ Now, if it’s the same company, they feel safer. It’s not perfect, but it’s a step toward trust.
Katie Schoen
Okay but imagine if ALL generics were made in the U.S. like this? No more supply chain chaos. No more ‘why is my blood pressure med backordered again?’
Yeah, the brand companies are still in charge… but if they’re making cheaper pills AND keeping them here? I’ll take it. 🙌
Ryan Barr
Manufacturing in the U.S. isn’t cheaper. It’s just politically convenient.
Stuart Shield
It’s like when your mate opens a second-hand shop next to his own boutique-same goods, different price tag. He’s not selling out, he’s just keeping the cash in the family. Smart? Yeah. Ethical? Hmm. But hey, the customer wins. That’s what matters, innit?
Indra Triawan
Is this not just capitalism’s final form? The system eats itself. The brand becomes the ghost of its own profit. We are all just nodes in a price matrix now. The pill doesn’t care who made it. Only the ledger does.
Lily Lilyy
Every step toward affordable, reliable medicine is a win for families across America. Let’s celebrate the fact that more people can access life-saving drugs-no matter who makes them. Thank you to the innovators, the regulators, and the pharmacists who make this possible. Keep pushing forward! 💪❤️
Susan Arlene
same pill different label same factory same everything why do we even have brands anymore
its just marketing with a side of regulation
Mukesh Pareek
You think this is transparent? The FDA’s pilot program is just another corporate subsidy disguised as nationalism. Real competition would require dismantling the ANDA system entirely. Until then, you’re just rearranging deck chairs on the Titanic of pharmaceutical monopolies.
Tom Swinton
Okay, let’s zoom out for a second. This isn’t just about pills-it’s about trust in the system. When you’ve been burned by a bad generic from overseas that didn’t work, and then you see your doctor’s brand-name drug suddenly available as a cheaper version… you feel relieved. Even if it’s the same company. Even if it’s the same factory. The psychological safety net matters. People aren’t just buying drugs-they’re buying peace of mind. And if that peace of mind comes from knowing the maker is the same one you’ve trusted for years? That’s not manipulation. That’s empathy in packaging. Plus, domestic production = fewer delays = fewer people missing doses. That’s a win. And yes, the brand companies are still in the game-but now they’re playing by rules that actually help patients. That’s evolution, not exploitation.
Harshit Kansal
so if i get my statin from merck but its labeled as simvastatin… does that mean i can still ask for the brand name and theyll give it to me? or am i just stuck with the generic version now? asking for a friend who’s paranoid about switching