Tramadol Risk Assessment Tool
Assess Your Risk of Serotonin Syndrome
This tool helps you understand your personal risk of developing serotonin syndrome when taking tramadol. Based on your medications, age, and health factors, you'll receive a personalized risk assessment and recommendations.
Most people think of opioids as drugs that dull pain by acting on opioid receptors in the brain. Morphine, oxycodone, hydrocodone - these are the classic examples. But tramadol doesn’t play by the same rules. It’s an opioid, yes, but it also messes with serotonin in ways that can turn a simple painkiller into a silent danger - especially when mixed with antidepressants or even taken alone at normal doses.
What Makes Tramadol So Unusual?
Tramadol was developed in the 1970s and approved in the U.S. in 1995. At first glance, it looks like any other pain med: it binds to opioid receptors to reduce pain signals. But here’s the twist - it also blocks the reuptake of serotonin and norepinephrine. That’s the same mechanism used by antidepressants like SSRIs and SNRIs. This dual action makes tramadol effective for nerve pain, but it also creates a risk most other opioids don’t have: serotonin syndrome.
Unlike morphine or fentanyl, which rarely cause serotonin syndrome even at high doses, tramadol can trigger it on its own. There are documented cases of people developing full-blown serotonin syndrome after taking just two 50 mg tablets - no other drugs involved. That’s not a fluke. It’s built into the drug’s chemistry.
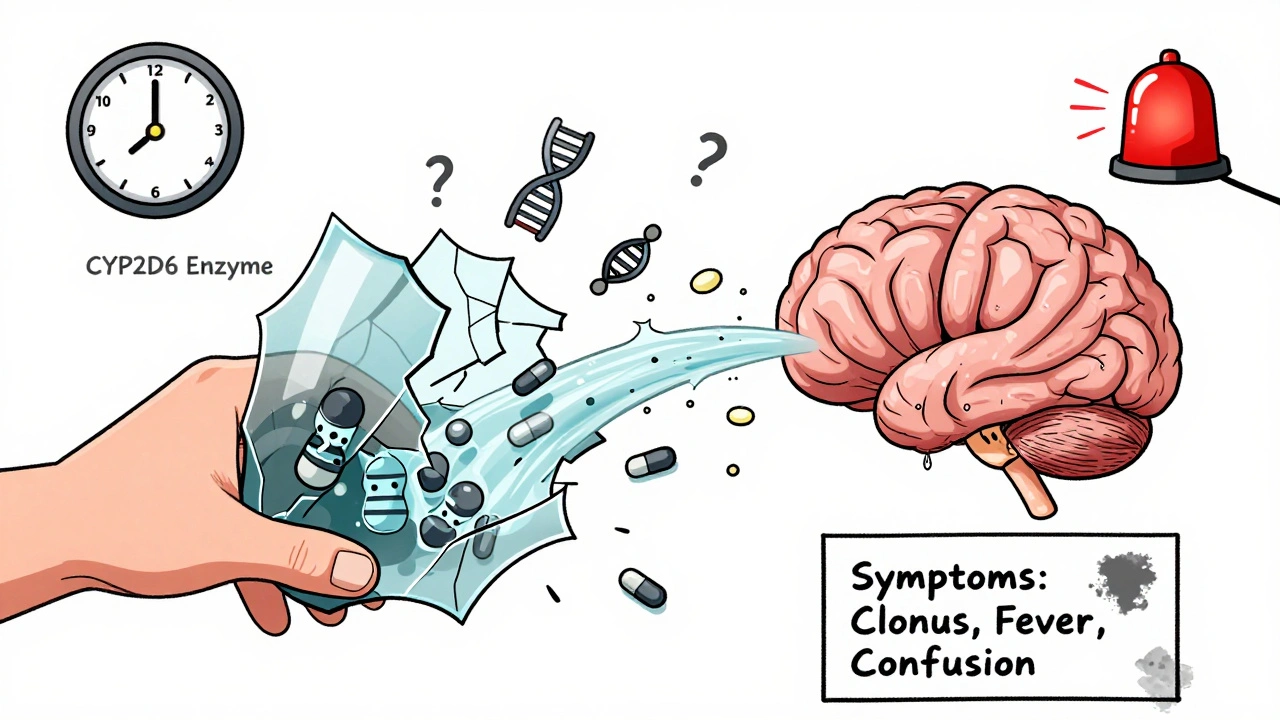
How Serotonin Syndrome Actually Happens
Serotonin syndrome isn’t just feeling a little jittery. It’s a potentially deadly condition caused by too much serotonin activity in the brain and spinal cord. Symptoms come on fast - sometimes within hours - and include:
- Clonus (involuntary muscle spasms, especially in the ankles)
- High fever (over 38°C or 100.4°F)
- Fast heartbeat and high blood pressure
- Heavy sweating
- Muscle rigidity
- Confusion, agitation, or hallucinations
The Hunter Serotonin Toxicity Criteria is the gold standard for diagnosis. You don’t need all these symptoms. Just one of these combinations is enough:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- Muscle rigidity + fever + clonus
Doctors miss this diagnosis all the time. Symptoms get mistaken for anxiety, infection, or even opioid withdrawal. A 2021 study estimated that only 28% of tramadol-related serotonin syndrome cases are correctly identified.
The Big Risk: Mixing With Antidepressants
The most dangerous scenario? Taking tramadol with an SSRI or SNRI - like fluoxetine (Prozac), sertraline (Zoloft), or venlafaxine (Effexor). These drugs already raise serotonin levels. Adding tramadol is like pouring gasoline on a fire.
A 2015 study of 187,000 Medicare patients found that combining tramadol with an SSRI increased serotonin syndrome risk by 3.6 times compared to taking the antidepressant alone. Another study showed a 14.7% incidence rate of serotonin syndrome with tramadol plus SSRIs - compared to less than 1% with codeine or hydrocodone.
Here’s the kicker: SSRIs also block the CYP2D6 enzyme, which is how your body breaks down tramadol. So when you take them together, tramadol builds up in your system faster than expected. You’re not just adding serotonin - you’re accidentally overdosing on tramadol.

Even Without Antidepressants, It Can Happen
You don’t need to be on an antidepressant for this to go wrong. About 7% of white people have a genetic variation that makes them poor metabolizers of tramadol. Their bodies can’t convert tramadol into its active pain-relieving form (M1) efficiently. That means more of the original tramadol - the part that blocks serotonin reuptake - stays in their system longer.
One case study described a 63-year-old woman who developed serotonin syndrome after taking the standard dose: 100 mg twice daily. No other drugs. Just tramadol. She had no history of depression. She didn’t know she was at risk. Her symptoms cleared up within 24 hours after stopping the drug - but she got lucky.
Another case involved a 35-year-old man who took 600 mg of tramadol with fluoxetine. His temperature hit 41.2°C (106.2°F). His heart rate was 142 beats per minute. He ended up in intensive care for three days. He survived. Many don’t.
Who Should Avoid Tramadol Altogether?
The American Geriatrics Society’s 2019 Beers Criteria lists tramadol as potentially inappropriate for older adults. Why? Older patients are more likely to have slowed metabolism, take multiple medications, and have undiagnosed depression. The risk of serotonin syndrome is 2.7 times higher in people over 65 compared to younger adults on other painkillers.
People with bipolar disorder are also at higher risk. There’s a documented case of a woman with bipolar II developing hypomania and serotonin syndrome just 48 hours after starting tramadol for fibromyalgia. Her mood shifted fast - and it was deadly.
Even if you’re not on antidepressants, if you’ve ever had depression, anxiety, or a history of serotonin-related side effects (like insomnia, agitation, or nausea from SSRIs), you should talk to your doctor before taking tramadol.
What Are the Alternatives?
If you need an opioid for pain but have depression or are on an antidepressant, there are safer options:
- Tapentadol - Works like tramadol but has minimal serotonin activity. A 2023 study found it caused 63% fewer cases of serotonin syndrome than tramadol.
- Morphine or oxycodone - Pure opioids with no serotonin effects. Safer if you’re on SSRIs.
- Non-opioid options - Gabapentin, pregabalin, or NSAIDs like naproxen may work for nerve pain without the risk.
For neuropathic pain, tramadol can still be effective - but only if you’re not on anything that boosts serotonin and you’re not a poor metabolizer. A 2023 meta-analysis found that 65% of diabetic neuropathy patients got 40-50% pain relief with tramadol at doses under 300 mg/day - as long as no interacting drugs were used.
What to Do If You Think You Have Serotonin Syndrome
Time matters. The sooner you stop tramadol and get treatment, the better your chances.
First: Stop taking tramadol immediately. Don’t wait to see if it gets better.
Second: Call emergency services or go to the ER. Don’t try to tough it out. Fever, confusion, and muscle rigidity can escalate quickly.
Third: Treatment is straightforward if caught early:
- Cyproheptadine - An antihistamine that blocks serotonin. First-line treatment. Usually 12 mg orally, then 2 mg every 2 hours until symptoms improve.
- Benzodiazepines - Like lorazepam or diazepam. Used to calm agitation and stop muscle spasms.
- Supportive care - Cooling blankets for fever, IV fluids, heart monitoring.
When treated within 6 hours, mortality drops from 22% to under 0.5%.
The Bigger Picture: Why Tramadol Is Still Prescribed
Despite the risks, tramadol is still widely used. In 2022, there were 39.4 million prescriptions in the U.S. - down from 43.2 million in 2018, thanks to growing awareness of its dangers.
The FDA added a black box warning in 2011 about seizure risk at doses over 400 mg/day. In 2014, it was reclassified as a Schedule II controlled substance, making it harder to get. Both moves cut down on misuse - but not necessarily on accidental serotonin syndrome.
Now, researchers are working on safer versions. A new compound called M1-tramadol is in Phase II trials. It keeps the pain-relieving effects but removes the serotonin-blocking action. And studies are testing CYP2D6 genetic testing before prescribing - so doctors can avoid giving tramadol to poor metabolizers.
The European Medicines Agency already says tramadol has an “unacceptable risk-benefit profile” for patients with psychiatric conditions. They may restrict its use by 2025.
Tramadol isn’t evil. It helps people. But it’s not a simple opioid. It’s a hidden risk - especially if you’re on antidepressants, have a history of mood disorders, or don’t know your metabolism type. If you’re prescribed tramadol, ask: Could this interact with what else I’m taking? And if you’re on an SSRI or SNRI - don’t assume it’s safe. It’s not.
Can tramadol cause serotonin syndrome by itself?
Yes. Unlike morphine or oxycodone, tramadol can cause serotonin syndrome even when taken alone at normal doses. Documented cases exist where people developed symptoms after taking just 100 mg twice daily with no other medications. This is due to its direct serotonin reuptake inhibition, not just its opioid effects.
Is tramadol safe if I’m on an SSRI like Zoloft?
No. Combining tramadol with SSRIs increases serotonin syndrome risk by 3.6 times. Both drugs raise serotonin levels, and SSRIs also block the enzyme (CYP2D6) that breaks down tramadol, leading to dangerous buildup. Most guidelines now say this combination should be avoided entirely.
What are the early warning signs of serotonin syndrome from tramadol?
Early signs include sudden muscle twitching (especially in the legs), unexplained sweating, restlessness, or feeling unusually anxious or confused. These can appear within hours of taking tramadol. If you’re on an antidepressant and notice these symptoms, stop the drug and seek help immediately.
Are there genetic tests to see if I’m at higher risk?
Yes. About 7% of white people are poor metabolizers of tramadol due to a CYP2D6 gene variation. This means they build up more of the serotonin-blocking form of the drug. Genetic testing is available and recommended by some pharmacists before starting tramadol, especially if you’ve had side effects from other medications.
What’s the safest painkiller if I’m on an antidepressant?
Tapentadol is the safest opioid alternative - it has little to no serotonin activity. For non-opioid options, gabapentin, pregabalin, or NSAIDs like naproxen may work depending on your pain type. Always discuss alternatives with your doctor before starting any new medication.
How long does it take for serotonin syndrome to go away after stopping tramadol?
Symptoms usually start improving within 24 hours of stopping tramadol. With proper treatment - like cyproheptadine and benzodiazepines - most people recover fully within 1-3 days. But without treatment, symptoms can worsen rapidly and become life-threatening.

Comments (15)
Eddie Bennett
I got prescribed tramadol last year for a herniated disc. Never knew it could do this. My doc never mentioned serotonin stuff. Scary stuff.
Michaux Hyatt
This is why I always ask my pharmacist about interactions. I'm on sertraline and was offered tramadol for back pain. They straight up said nope, try tapentadol instead. Saved me from a potential nightmare.
Jack Appleby
The fact that the FDA didn't act sooner on this is criminal. Tramadol's dual pharmacology was well-documented in the 90s. This isn't some new discovery-it's negligence dressed up as "off-label use."
Sylvia Frenzel
Americans are so quick to pop pills. In Europe they already banned this junk. We're still letting doctors hand it out like candy.
Raj Rsvpraj
I'm Indian, and we've had this problem for years-doctors here prescribe tramadol like it's aspirin. No genetic testing, no counseling. People die because no one cares. It's not a "Western problem," it's a global failure.
Sarah Clifford
So basically tramadol is just a sneaky antidepressant with painkillers attached? Why not just take the real thing and save the risk?
Regan Mears
I had clonus after a 100mg dose. Thought I was having a seizure. ER said "probably serotonin." Doc just shrugged. I stopped it cold turkey. Never touched it again. This needs to be on every prescription label.
Frank Nouwens
The Hunter Criteria are underutilized in clinical practice. Emergency departments often misattribute symptoms to anxiety or infection. Standardized screening protocols are urgently needed.
Ben Greening
I'm a pharmacist. I see this every week. Patients don't know their meds interact. They think "it's just a painkiller." We need mandatory counseling when tramadol is prescribed.
Aileen Ferris
I took tramadol for a month after surgery. Felt weirdly wired but thought it was just the pain meds. Turns out I was lowkey serotonin poisoning. My doc said I was lucky. I wasn't lucky. I was clueless.
David Palmer
I'm bipolar and was on fluoxetine. Doc gave me tramadol for migraines. Two days later I was in mania mode, sweating, shaking, couldn't sleep. They thought I was just "relapsing." Took me months to get them to listen. This needs to be common knowledge.
john damon
I'm not mad at the post. I'm mad at the system. Why is this drug still on the market? It's like they gave a kid a loaded gun and said "don't point it at your head."
Michelle Edwards
If you're on any antidepressant, please, please, please talk to your doctor before taking anything new. I used to think "it's just one pill"-now I know better. You're worth more than a risky shortcut.
matthew dendle
So basically tramadol is just a chemical trap for people who dont read the fine print? Wow. And we wonder why people dont trust doctors
Jim Irish
I'm a retired nurse. We used to joke about tramadol being "SSRI lite." Now I wish we'd taken it more seriously. This isn't just a drug-it's a silent landmine.