Urination Difficulty: What’s Going On and What You Can Do
Struggling to pee, feeling like you can’t fully empty your bladder, or having pain when you go—these are all types of urination difficulty. It’s common and usually fixable, but some patterns need quick medical care. Below you’ll find clear, practical steps, simple home tips, and signs that mean you should see a doctor now.
Common causes and quick checks
Start by asking a few short questions: Is there pain? Fever? Blood in the urine? Are you passing any urine at all? These help narrow things down.
Typical causes include:
- Urinary tract infection (UTI) — often burning, urgency, cloudy or strong-smelling urine.
- Enlarged prostate (BPH) in men — weak stream, dribbling, feeling of incomplete emptying.
- Urinary retention — can be sudden and total (an emergency) or partial.
- Medications — some antihistamines, decongestants, antidepressants, anticholinergics, and opioids can make it hard to pee.
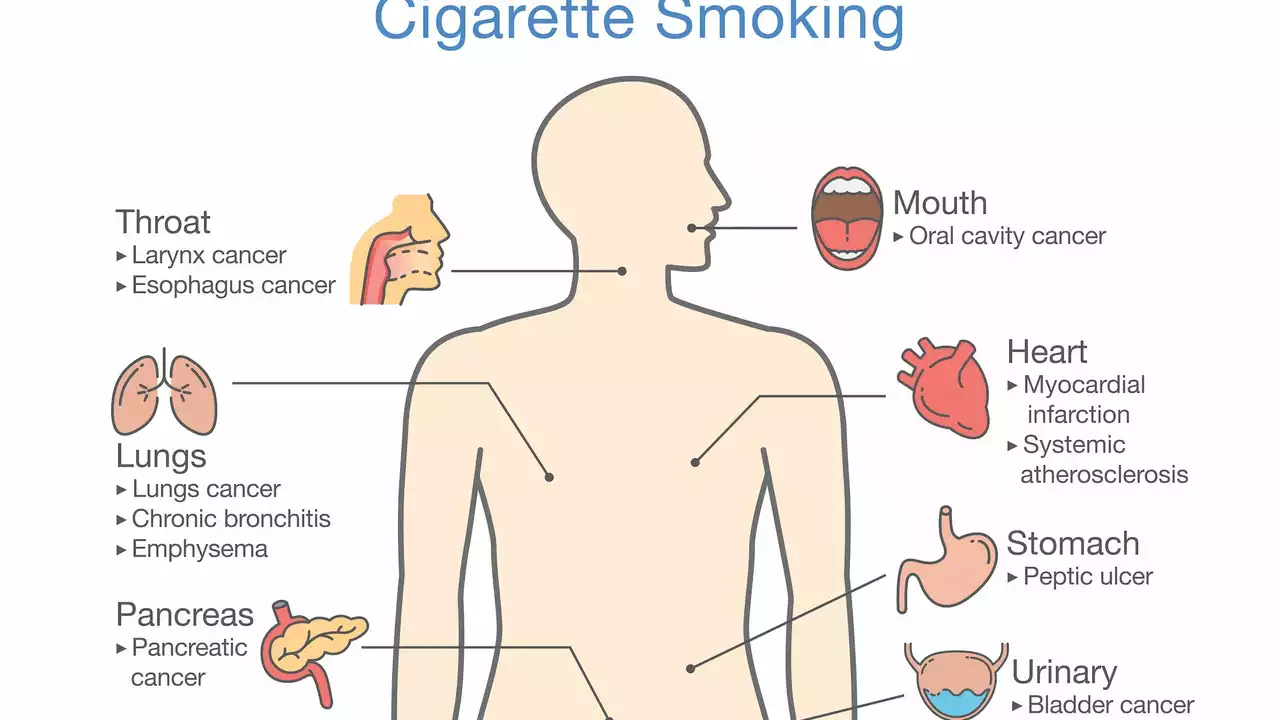
- Bladder or urethral obstruction — stones, strictures, or tumors can block flow.
- Neurologic causes — diabetes, spinal problems, or nerve disorders affect bladder signals.
What to do now: practical steps and common treatments
If you can pass urine but it’s uncomfortable, try these immediate steps:
- Drink plain water steadily—don’t chug—and avoid alcohol, caffeine, and spicy foods for 24–48 hours.
- Sit in a warm bath or place a warm compress over the lower belly to relax muscles.
- Try double voiding: pee, wait a few minutes, then try again to empty more fully.
- Check your meds. If a new drug started your symptoms, ask your prescriber if it could be the cause.
If symptoms don’t improve in 24–48 hours, make a medical appointment. Common tests your clinician may use include a urine dipstick and culture, bladder scan for residual urine, ultrasound, and sometimes blood tests.
Treatments depend on the cause: antibiotics for UTIs, alpha-blockers (like tamsulosin) for prostate-related blockage, short-term catheterization for acute retention, or referral to urology for further investigation. Pelvic-floor therapy helps many women with weak or too-tight pelvic muscles.
Bring a short log to your visit: when symptoms started, how often you go, how much you pass, any fever, and a full list of medicines. That saves time and helps get the right treatment faster.
Urgent warnings: Go to the ER now if you can’t pass any urine at all, have severe lower belly pain, high fever, or vomiting. These are signs of acute retention or a serious infection and need immediate care.
If your symptoms are mild, quick home care plus a prompt checkup will usually sort it out. If you’re unsure, call your clinic—early action prevents complications and gets you back to normal faster.