Pediatric Hepatitis C: What Parents Need to Know
Pediatric hepatitis C often comes from mother-to-child transmission at birth, but many children have no symptoms and do well for years. That makes testing and clear follow-up important because modern treatments can cure the infection and prevent long-term liver damage.
If you’re worried your child was exposed, here's what doctors usually do: babies born to HCV-positive mothers can be tested with an HCV RNA (PCR) test at about 2–6 months of age. Maternal antibodies can last up to 18 months, so an antibody test is usually done after 18 months to confirm whether the child truly cleared or has chronic infection. Older children who had blood exposure, IV drug use, or other risks should be screened with antibody tests and PCR as needed.
Most kids with hepatitis C look and feel fine. When symptoms appear they can include tiredness, poor weight gain, belly pain, jaundice (yellow skin or eyes), and dark urine. These signs are not specific, so testing is the only reliable way to know.
Transmission in children is mainly perinatal. Rarely it spreads through shared needles, blood contact, or inadequately sterilized medical equipment. Breastfeeding is generally safe unless the mother has cracked or bleeding nipples; discuss this with your pediatrician. Simple prevention at home includes avoiding sharing razors or toothbrushes and ensuring any blood spills are cleaned promptly.
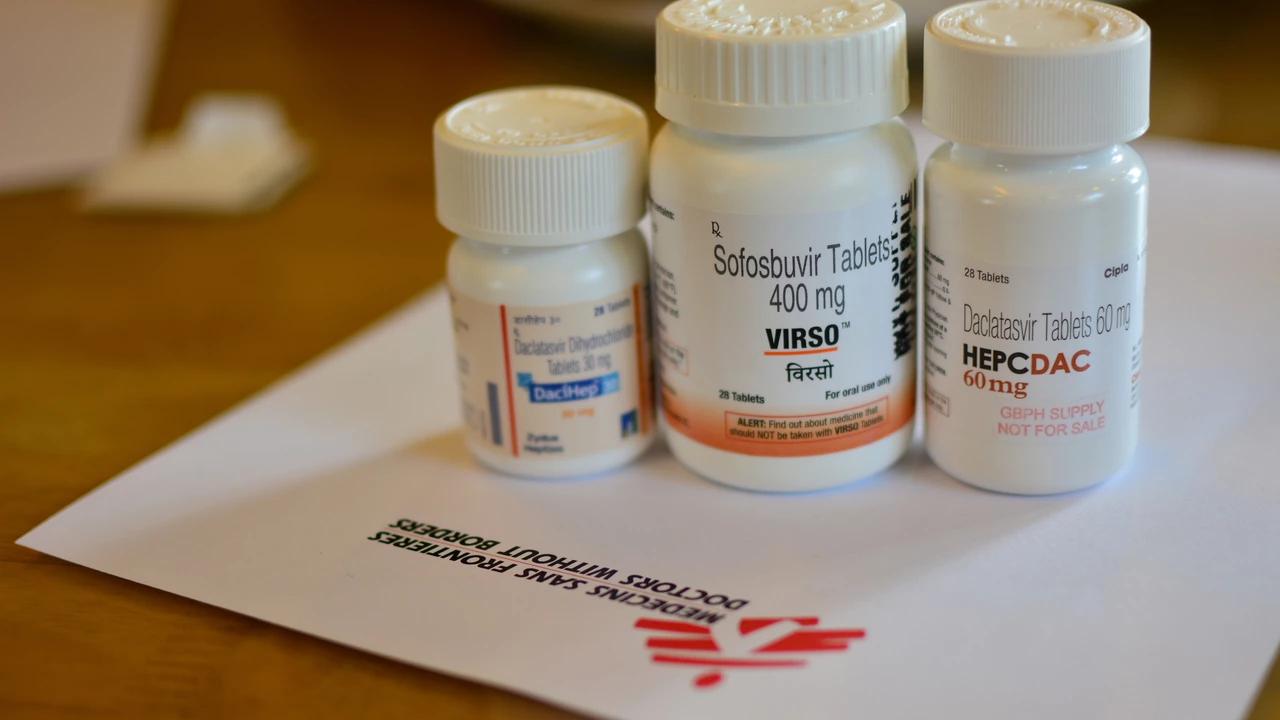
Treatment has changed a lot in recent years. Direct-acting antivirals (DAAs) are oral pills that cure most children with hepatitis C, often with 8–12 week courses. Which drug is right depends on the child’s age, weight, virus type, and other health issues. Pediatric specialists will pick the right regimen and dose. Side effects are usually mild, but regular follow-up during treatment is standard.
While waiting for testing or treatment, protect the child’s liver. Keep vaccinations up to date — hepatitis A and B vaccines are recommended if not immune. Avoid unnecessary medicines or supplements that can harm the liver, and check with your doctor before giving over-the-counter drugs like extra-strength acetaminophen or herbal products.
Follow-up matters. Even after a cure, doctors may check liver blood tests and sometimes imaging for children who had advanced disease. If your child has other conditions — like HIV or inherited liver disease — care teams coordinate treatment.
Practical steps now: if you know the mother is HCV-positive, ask the pediatrician for an HCV RNA test at the recommended time. Keep medical records handy, ask about pediatric hepatology referral, and write down questions before visits. Treatment is much simpler than it used to be, and a timely test can change the outcome for your child.
Insurance and cost questions are common. Many insurance plans and programs cover pediatric DAA treatment, but prior authorization can be required. Ask your clinic to help with paperwork and patient-assistance programs. Schools do not need to exclude a child with hepatitis C; check with your doctor about first-aid protocols. If you feel overwhelmed, ask for a social worker or support group referral today.