When a rheumatologist prescribes Humira instead of a biosimilar, or an oncologist chooses Ocrevus over a cheaper alternative, it’s not because they’re ignoring cost. It’s because they’ve seen what happens when patients switch.
Specialty drugs aren’t your regular pills you pick up at the corner pharmacy. These are high-cost, complex medications used for serious, often rare conditions-cancer, multiple sclerosis, rheumatoid arthritis, Crohn’s disease. They’re injected or infused. They need special storage. They require constant monitoring. And they’re expensive: more than half cost over $100,000 a year per patient. Yet despite the price tag, specialists keep reaching for the brand-name version-even when generics or biosimilars are available.
Why brand-name drugs still dominate specialty care
The numbers tell a stark story. In 2021, specialty drugs made up just 6.2% of all prescriptions in the U.S., but they accounted for 71.1% of total prescription drug spending. That’s not a typo. Less than one in twenty prescriptions drove over seven in ten dollars spent on medications.
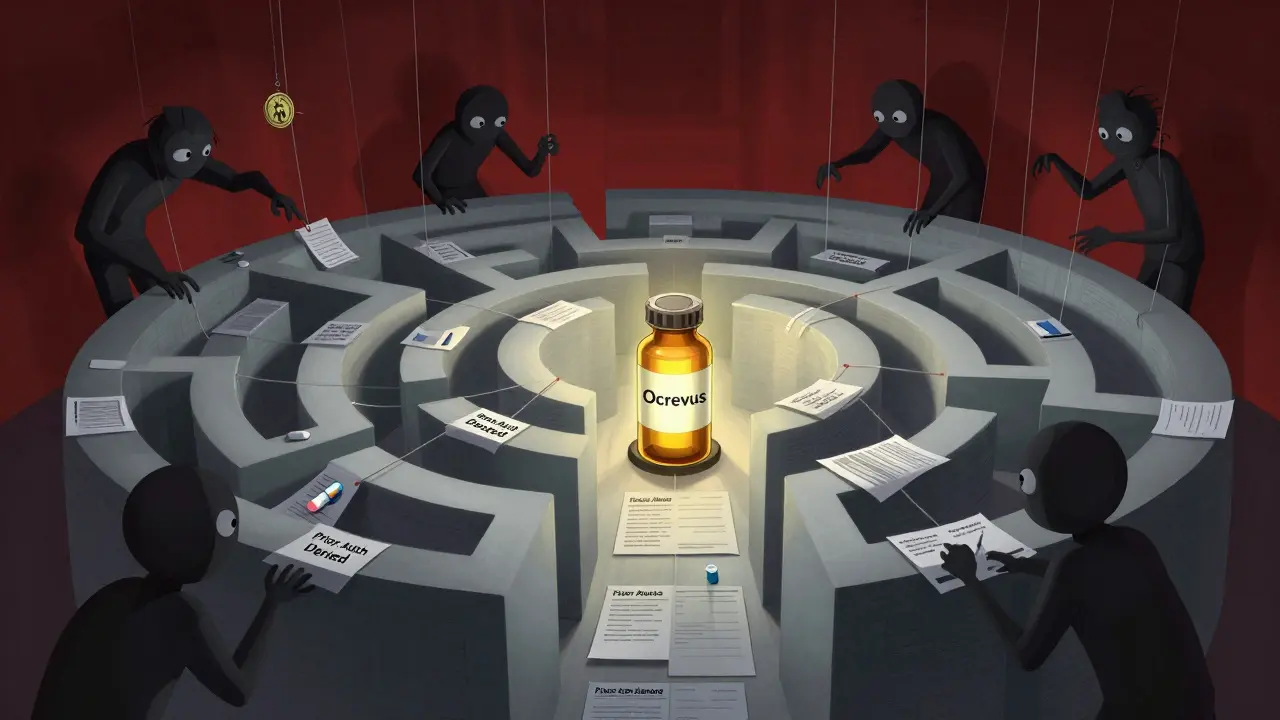
Why? For many of these conditions, there are no good alternatives. Take multiple sclerosis. Ocrevus (ocrelizumab) is a brand-name drug. A biosimilar exists-but many neurologists won’t switch their patients. Why? Because the disease is unpredictable. A small change in how the immune system responds can trigger a relapse. Doctors aren’t gambling with someone’s ability to walk, see, or breathe just to save a few thousand dollars.
One 2023 Medscape survey found that 68% of specialists felt frustrated by prior authorization delays for specialty drugs. Oncologists and rheumatologists reported even higher rates-82% and 79%, respectively. These aren’t bureaucratic annoyances. They’re delays in life-saving treatment. When a patient’s insurance denies a biosimilar because it’s not on formulary, the doctor has to appeal. That takes weeks. In cancer care, weeks matter.
The role of patient and provider experience
It’s not just about clinical data. It’s about real-world outcomes. A patient on Humira for years might have stable disease. Switching to a biosimilar? Maybe it works. Maybe it doesn’t. And if it doesn’t? The patient could end up in the hospital. That’s not just a health risk-it’s a financial risk for the practice. Reimbursement rates for specialty drugs are already tight. A hospitalization due to a switch can wipe out margins.
On Reddit’s r/healthinsurance, a user named u/ChronicWarrior42 wrote: “I pay $1,200 a month for Ocrevus-even with insurance. My specialist says there are no alternatives that work as well for my specific mutation.” That’s not an outlier. It’s a common refrain among patients with rare conditions.
Doctors aren’t blind to cost. They see the bills. But they also see the patients who’ve tried generics and ended up worse. In one study, prescriber or patient requests for brand-name drugs over generics added $1.67 billion in costs to Medicare in a single year. That’s not because doctors are greedy. It’s because they’ve learned, often the hard way, that “cheaper” doesn’t always mean “safer.”
The hidden drivers: PBMs and pricing distortion
Here’s the twist: the system isn’t designed to help doctors choose the best drug. It’s designed to profit from complexity.
Pharmacy Benefit Managers (PBMs)-the middlemen between insurers, pharmacies, and drugmakers-control 68% of specialty drug dispensing in the U.S. According to the FTC’s January 2025 report, PBMs marked up specialty generic drugs by thousands of percent. One drug with a $500 acquisition cost was dispensed for $18,000. That’s not inflation. That’s a system rigged to reward opacity.
When a PBM owns a specialty pharmacy, they profit more from brand-name drugs. Why? Because they can charge higher rebates and markups. Biosimilars? Lower price. Lower profit. So even if a biosimilar is clinically equivalent, the system pushes the brand. And doctors? They’re caught in the middle.
Dr. Peter Bach from Memorial Sloan Kettering put it bluntly: “The current system allows manufacturers to set prices without meaningful competition.” That’s especially true in specialty care, where there’s often only one or two drugs that work.
What about payments from drug companies?
ProPublica’s 2016 analysis found that doctors who received over $5,000 from pharmaceutical companies in 2014 prescribed brand-name drugs at a rate 50% higher than those who received nothing. That’s a correlation-but is it causation?
It’s not that every specialist is swayed by free dinners or speaker fees. But the data shows a pattern: financial ties correlate with prescribing habits. And in specialty care, where margins are thin and pressure is high, those relationships matter more than we admit.
One rheumatologist in Texas told a reporter, “I don’t take payments. But I know which reps know the ins and outs of patient assistance programs. If I can get a patient on a $0 copay with the brand, I’m going to do it. Not because I like the company. Because I don’t want them to drop treatment.”
The administrative nightmare
Prescribing a specialty drug isn’t just writing a prescription. It’s a full-time job.
Physicians spend an average of 13.4 hours a week just on prior authorizations-and 78% of that time is spent on specialty drugs. That’s 13.4 hours they’re not spending with patients. Not reviewing labs. Not researching new treatments. Just filling out forms, calling insurers, appealing denials.
And it’s not getting easier. A 2024 JMCP study found that 42% of specialty drug starts are delayed by seven or more days due to administrative hurdles. For a patient with aggressive MS or advanced cancer, that delay can mean disease progression.
Specialty pharmacies require enrollment. REMS programs (Risk Evaluation and Mitigation Strategies) need documentation. Patient support services must be coordinated. And not every manufacturer provides clear guidelines. The FDA found in 2023 that only 65% of specialty drug makers gave comprehensive REMS instructions.
What’s changing-and what’s not
The Inflation Reduction Act of 2022 let Medicare negotiate prices for some high-cost drugs. That’s a start. Drugs like Jakafi, Ofev, and Xtandi are already on the list for future negotiation.
But the real problem isn’t just drug prices. It’s the entire supply chain. PBMs still control distribution. Markups are still hidden. Biosimilars are still treated like second-class options-even when they’re proven safe.
Some states are stepping in. California and New York have passed laws requiring PBM transparency. But without federal action, it’s a patchwork. And specialists? They’re still prescribing the same drugs, for the same reasons: because they’ve seen what happens when you try to cut corners.
It’s not about loyalty. It’s about risk.
Specialists don’t prefer brand-name drugs because they’re loyal to Pfizer or Roche. They prefer them because their patients have lived through the alternatives-and didn’t survive the switch.
They know the cost. They see the numbers. But they also see the person sitting across from them. And when the stakes are this high, they choose what they know works.
The system is broken. But until the pricing, the markups, and the administrative chaos are fixed, doctors will keep writing those expensive prescriptions. Not because they want to. But because they have to.


Comments (10)
Alvin Bregman
Doctors aren't greedy they're just tired of watching people die because some bean counter thinks $50k is too much to pay for a drug that keeps someone alive
we act like it's a choice but it's not
Henry Sy
PBMs are the real villains here not the docs
they turn a $500 drug into $18k and then act shocked when doctors stick with the brand
its not loyalty its survival
and dont even get me started on how they own the specialty pharmacies so they profit more from the expensive stuff
this system is a fucking carnival ride rigged by accountants in suits
Robert Way
my cousin got switched to a biosimilar for her ms and she had a relapse within 3 weeks
they had to rush her to the hospital
now they wont let her switch back because insurance says its too risky
so shes stuck paying 1200 a month for the brand
and the doc just shrugs
he says he saw this coming
Vicky Zhang
it breaks my heart to see how hard doctors have to fight just to give their patients the meds they need
they spend more time on paperwork than with people
and then people blame them for the cost
but its not their fault
theyre just trying to keep someone alive
theyre not the ones making the rules
theyre the ones stuck cleaning up the mess
we need to fix the system not punish the healers
Allison Deming
It is profoundly irresponsible to continue prescribing high-cost pharmaceuticals without exhaustive evidence of comparative effectiveness, particularly when biosimilars have undergone rigorous FDA review.
Physicians who prioritize convenience over evidence-based practice are not only ethically compromised but also contribute to systemic fiscal irresponsibility that ultimately harms public health.
The notion that patient anecdotes outweigh clinical trials is a dangerous fallacy that has no place in modern medicine.
Furthermore, the reliance on anecdotal evidence undermines the scientific integrity of our healthcare system and sets a perilous precedent for future treatment paradigms.
Susie Deer
usa healthcare is broken but dont blame the doctors
blame the politicians who let pbms run wild
we need to burn the whole system down and start over
no more middlemen
no more markups
no more excuses
if you want to save lives stop letting corporations profit off suffering
TooAfraid ToSay
you think this is unique to america?
in nigeria we dont even have access to the brand name drugs
so we get generics or nothing
and you people are mad because doctors here dont want to gamble with people's lives?
you're not fighting for fairness you're fighting for your privilege
get a grip
Dylan Livingston
oh look another sanctimonious tirade about how doctors are saints
let me guess you also think they don't take free dinners and kickbacks
and that the $1.67 billion in unnecessary medicare spending is just a myth
please
the system is rigged but the doctors are not innocent bystanders
they're beneficiaries
they know exactly how much they profit from keeping things the way they are
and they're not about to give that up just because someone's MS relapsed
Andrew Freeman
the real problem is no one talks about how pbms own the pharmacies
so when they push the brand name drug they make more money
the doc doesnt even have to be bribed
the system just works that way
its like a vending machine that only gives you the expensive candy
you dont have to be corrupt to be complicit
says haze
the emotional appeal here is seductive but intellectually bankrupt
we are not dealing with a moral dilemma we are dealing with a structural failure of market design
the conflation of clinical caution with ethical virtue obscures the deeper issue: the absence of price elasticity in specialty pharmaceuticals
doctors are not heroes they are agents of a broken incentive structure
and until we dismantle the PBM-monopoly nexus and introduce true competition we are merely romanticizing the symptoms of systemic rot
the patient's suffering is real but so is the complicity of the system that commodifies their vulnerability