NSAID-Blood Thinner Risk Calculator
Select Medications
Risk Assessment
Select medications to see risk assessment
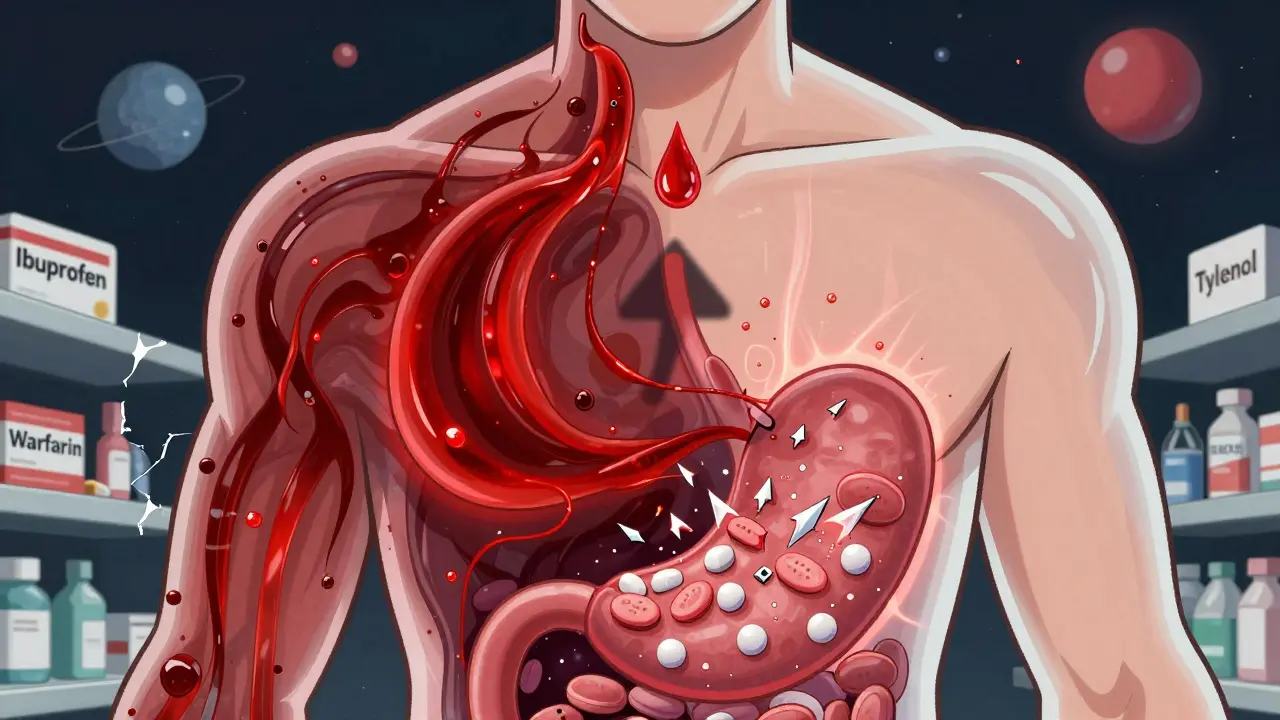
Every year, millions of people take NSAIDs like ibuprofen or naproxen to manage everyday pain-arthritis, backaches, headaches. At the same time, over 12 million Americans over 65 are on blood thinners to prevent strokes or clots. What happens when these two commonly used medications cross paths? The answer isn’t just a warning label. It’s a real, measurable, and often deadly risk that many people don’t even know they’re taking.
Why This Combination Is So Dangerous
NSAIDs and blood thinners don’t just work separately-they amplify each other’s risks. NSAIDs block enzymes called COX-1 and COX-2. That’s how they reduce inflammation and pain. But COX-1 also helps protect your stomach lining and keeps platelets sticky enough to form clots when needed. When you take an NSAID, your platelets can’t do their job as well. Meanwhile, blood thinners like warfarin, rivaroxaban, or apixaban work by thinning your blood, making it harder for clots to form. Put them together, and your body loses two layers of protection against bleeding.This isn’t theoretical. A 2024 study from Denmark tracked over 200,000 patients on blood thinners. Those who also took NSAIDs had more than double the risk of serious bleeding. Some NSAIDs were far worse than others. Naproxen increased bleeding risk by 4.1 times. Diclofenac? That jumped to 3.3 times. Even common ibuprofen raised the risk by nearly 80%.
Where the Bleeding Happens
Bleeding doesn’t just mean a cut that won’t stop. When NSAIDs and blood thinners mix, the damage often happens inside your body-where you can’t see it.- Gastrointestinal bleeding: This is the most common. NSAIDs erode the stomach lining. Blood thinners prevent clots from sealing the damage. Together, they cause ulcers, internal bleeding, and anemia. The risk goes up by over 2 times.
- Intracranial hemorrhage: Bleeding in the brain. The risk jumps 3.2 times higher when NSAIDs are taken with anticoagulants. A single fall or minor head bump can turn life-threatening.
- Pulmonary and urinary bleeding: Less common, but still dangerous. Blood in the lungs or urine can be silent until it’s severe.
One patient in a 2023 FDA report took ibuprofen for a toothache while on apixaban. He bled internally for three days before collapsing. He needed a blood transfusion and a 10-day hospital stay. He didn’t know the two drugs could interact.
Not All Blood Thinners Are Equal
The risk isn’t the same across every blood thinner. Warfarin, the older drug, interacts more strongly with NSAIDs. Studies show warfarin + NSAID users have a 3.8 times higher bleeding risk. Newer drugs like apixaban and rivaroxaban are safer-but not safe. Even with DOACs (direct oral anticoagulants), NSAIDs still double the risk.Why does warfarin react worse? Because NSAIDs can push your INR (a measure of blood clotting time) up by 0.8 to 1.2 points. That’s enough to push you out of the safe range. With DOACs, the interaction is less about lab numbers and more about how NSAIDs directly weaken platelet function. Either way, the outcome is the same: too much bleeding.
The Only Safe Painkiller? Acetaminophen
If you’re on a blood thinner and need pain relief, there’s one clear alternative: acetaminophen (Tylenol). Unlike NSAIDs, it doesn’t affect platelets or the stomach lining. Multiple studies confirm it doesn’t raise bleeding risk when taken with warfarin or DOACs-as long as you stay under 4,000 mg per day.But it’s not perfect. Too much acetaminophen can damage your liver. That’s a real concern for older adults or those with existing liver problems. Still, for most people, it’s the safest bet. And it works for headaches, joint pain, and fever. The trade-off? It doesn’t reduce inflammation like NSAIDs do. But for someone on blood thinners, that’s a small price to pay.

What About Celecoxib? Is It Safer?
Celecoxib (Celebrex) is a COX-2 inhibitor, marketed as a “gentler” NSAID because it doesn’t hit COX-1 as hard. That means less stomach damage. But here’s the catch: it still affects platelets enough to raise bleeding risk when combined with blood thinners. Studies show it still increases bleeding by 1.4 times. That’s better than naproxen, but still too risky to recommend.There’s no “safe NSAID” for someone on a blood thinner. Only “less dangerous.” And even that’s not worth the gamble.
Real People, Real Mistakes
Online forums tell a grim story. On Reddit’s r/Anticoagulants, 62% of 1,457 users admitted to taking NSAIDs with their blood thinners. Nearly 4 out of 10 had bleeding episodes-nosebleeds, bruising, dark stools. One man took ibuprofen before a dental cleaning. He bled for hours. His dentist didn’t ask about his meds. His pharmacist didn’t flag it. He didn’t think to tell them.Another common trap? Cold medicines. Many contain ibuprofen or naproxen under “pain reliever” or “fever reducer.” Patients don’t read labels. They think, “It’s just a cold pill.”
And then there’s the dentist. A 2022 study found that 15% of emergency cases involving DOACs and NSAIDs started with a dentist prescribing ibuprofen after a procedure-without checking the patient’s anticoagulant status.
How to Stay Safe
If you’re on a blood thinner, here’s what you need to do:- Avoid all NSAIDs. That includes aspirin (unless it’s prescribed for heart protection), ibuprofen, naproxen, diclofenac, and celecoxib.
- Use acetaminophen instead. Stick to 3,000-4,000 mg per day. Don’t exceed it.
- Check all OTC labels. Look for “ibuprofen,” “naproxen,” “ketoprofen,” or “NSAID” on cold, flu, or headache pills.
- Talk to your pharmacist. Every time you fill a prescription, ask: “Does this interact with my blood thinner?”
- Ask about alternatives. Physical therapy, heat packs, or topical creams (like diclofenac gel) may help joint pain without systemic risk.
For those who absolutely must use an NSAID-for example, after a short-term injury-the guidelines are strict: use the lowest dose (ibuprofen ≤400 mg/day), for no more than 3 days, and always with a stomach-protecting drug like pantoprazole. Even then, it’s risky.

Why Doctors Miss This
You’d think hospitals would have systems to catch this. But only 38% of U.S. hospitals have electronic alerts that block prescriptions when NSAIDs and blood thinners are ordered together. Most rely on doctors remembering. And they don’t always.A 2023 study in JAMA Internal Medicine found only 29% of patients remembered being warned about NSAID risks three months after their doctor told them. Another 42% needed a pharmacist to explain it clearly. Polypharmacy-taking seven or more medications-is common in older adults. One drug gets lost in the pile.
The Cost of Ignoring the Risk
This isn’t just about individual harm. It’s a national crisis. In the U.S. alone, NSAID and blood thinner interactions cause:- 87,000 emergency room visits each year
- 24,000 hospitalizations
- $1.2 billion in annual healthcare costs
And it’s preventable. Hospitals with dedicated anticoagulant stewardship programs cut inappropriate NSAID use by 37%. That’s 37% fewer bleeding events, fewer deaths, fewer bills.
What’s Coming Next
The FDA is working on AI tools that will automatically flag NSAID prescriptions for patients on blood thinners. Early tests show 85% accuracy. The American Heart Association’s 2025 guidelines will likely make warnings even stronger, citing new data that shows this combo increases death risk by 1.8 times.Meanwhile, researchers are testing time-separated dosing-taking the NSAID 8 hours apart from the blood thinner. Early trials showed a 29% drop in bleeding. But until that’s proven safe and widely adopted, the only sure thing is avoidance.
By 2030, experts predict half of all NSAID prescriptions for patients on blood thinners will disappear-thanks to better alerts, better education, and better alternatives. But right now? The danger is real. And it’s still happening every day.
Can I take ibuprofen with warfarin?
No. Combining ibuprofen with warfarin significantly increases your risk of dangerous bleeding, especially in the stomach and brain. Studies show this combination raises bleeding risk by nearly 4 times. Even occasional use can be risky. Acetaminophen (Tylenol) is the safer pain relief option.
Is aspirin safe with blood thinners?
Aspirin is an NSAID and also thins the blood by affecting platelets. Unless your doctor specifically prescribed low-dose aspirin for heart protection, you should not take it with any other blood thinner. Combining them increases bleeding risk without proven benefit for most people.
What pain reliever is safe with apixaban?
Acetaminophen (Tylenol) is the safest choice. It does not interfere with blood clotting or stomach lining protection. Stick to 3,000-4,000 mg per day. Avoid all NSAIDs, including ibuprofen, naproxen, and diclofenac-even in small amounts or short-term use.
Can I use topical NSAID creams if I’m on blood thinners?
Topical NSAIDs like diclofenac gel are absorbed in much smaller amounts than pills. Some studies suggest they’re safer, but there’s still a risk. Most experts recommend avoiding them unless approved by your doctor. Acetaminophen or physical therapy are still the preferred options.
Why don’t pharmacies always warn me about this?
Many pharmacies don’t have automated alerts for this interaction, and pharmacists are often overwhelmed. Over-the-counter NSAIDs are sold without prescriptions, so there’s no system to flag them. Always ask your pharmacist directly: “Is this safe with my blood thinner?” Don’t assume they’ll tell you.

Comments (11)
Ojus Save
lol i just took ibuprofen for my back pain last week and im on warfarin... hope i dont bleed out lol
jk kinda. but seriously, i had no idea this was a thing. my dr never mentioned it.
Sonja Stoces
THIS IS WHY WE CAN'T HAVE NICE THINGS 😤
Everyone thinks OTC means 'safe' like it's some kind of vitamin. NSAIDs are just slow poison with a smiley face on the bottle. And don't even get me started on how pharmacists are too busy scanning barcodes to care. 😒
My grandma almost died because she took 'just one' naproxen for her knee. Turns out 'just one' is all it takes when you're on apixaban. #DontBeThatPerson
Rachidi Toupé GAGNON
Acetaminophen is the real MVP here 🙌
Simple, effective, doesn't turn your insides into a leaky faucet. I've been switching everyone I know over to it - moms, grandpas, even my buddy who thinks Tylenol is 'weak'.
It’s not flashy but it saves lives. And yeah, liver’s a thing - but so is bleeding out in the bathroom at 3am. 🤷♂️
Sophia Nelson
I'm sorry but this article is so alarmist. Everyone's panicking over 'bleeding risk' like it's a horror movie. I've been on Xarelto for 5 years and took ibuprofen twice. No issues. Maybe I'm just lucky?
Craig Staszak
i think the real issue here is that we treat meds like candy
you grab a pill because it hurts and you don't think about the domino effect
the system's broken. drs are rushed, pharmacists are swamped, and patients are just trying to feel better
we need better warnings. not more fear
alex clo
While the data presented is compelling, it is imperative to acknowledge that individual patient risk profiles vary significantly. The generalization of 'avoid all NSAIDs' may not be clinically appropriate for every individual, particularly when alternative therapies are insufficient. A nuanced, case-by-case approach guided by pharmacogenomic and comorbidity data is recommended.
Ernie Simsek
i took naproxen for a headache last month and my gums started bleeding like a faucet 😳
thought it was just brushing too hard
turns out i was on rivaroxaban and didn't connect the dots
now i only use tylenol and i'm a changed man
seriously though - read the tiny print. it's there for a reason.
Kristin Jarecki
The evidence supporting acetaminophen as the safest analgesic in patients on anticoagulants is robust and consistently replicated across multiple observational cohorts. However, it is critical to emphasize that hepatotoxicity remains a non-negligible concern in patients with pre-existing liver disease, chronic alcohol use, or concomitant use of other hepatically metabolized medications. A comprehensive medication reconciliation is essential prior to any analgesic recommendation.
Steve DESTIVELLE
you know what this really is? a failure of human connection
we live in a world where we are told to trust machines and doctors and pharmacists
but no one sits with you and says 'listen, your body is a fragile house and these pills are like keys that open doors you didn't know existed'
we are not taught to listen to our bodies
we are taught to pop pills and move on
and that's why people die quietly in their bathrooms
not because they're stupid
because no one taught them to care enough to ask
Gabriella Adams
I'm so glad this got attention. My mom had a GI bleed last year after taking diclofenac for arthritis. She didn't even realize it was an NSAID - it was just 'that cream the physio gave me.'
Now she uses heat wraps, physical therapy, and acetaminophen - and she's thriving.
Education is everything. I've started telling everyone I know: 'If it says NSAID on it, don't touch it.'
Jim Johnson
just a quick heads up - if you're on blood thinners and you're thinking about using a topical NSAID gel? don't. i know it sounds harmless but your skin absorbs more than you think. my uncle got a bleed from diclofenac cream. he thought it was 'just a cream'...
tylenol is your friend. keep it simple. stay safe. 💪