QT Interval Calculator for Methadone Patients
QT Interval Assessment Tool
Enter your ECG measurements to calculate corrected QT interval (QTc) and assess cardiac risk related to methadone therapy.
Results
Why Methadone Can Slow Your Heart’s Electrical Signal
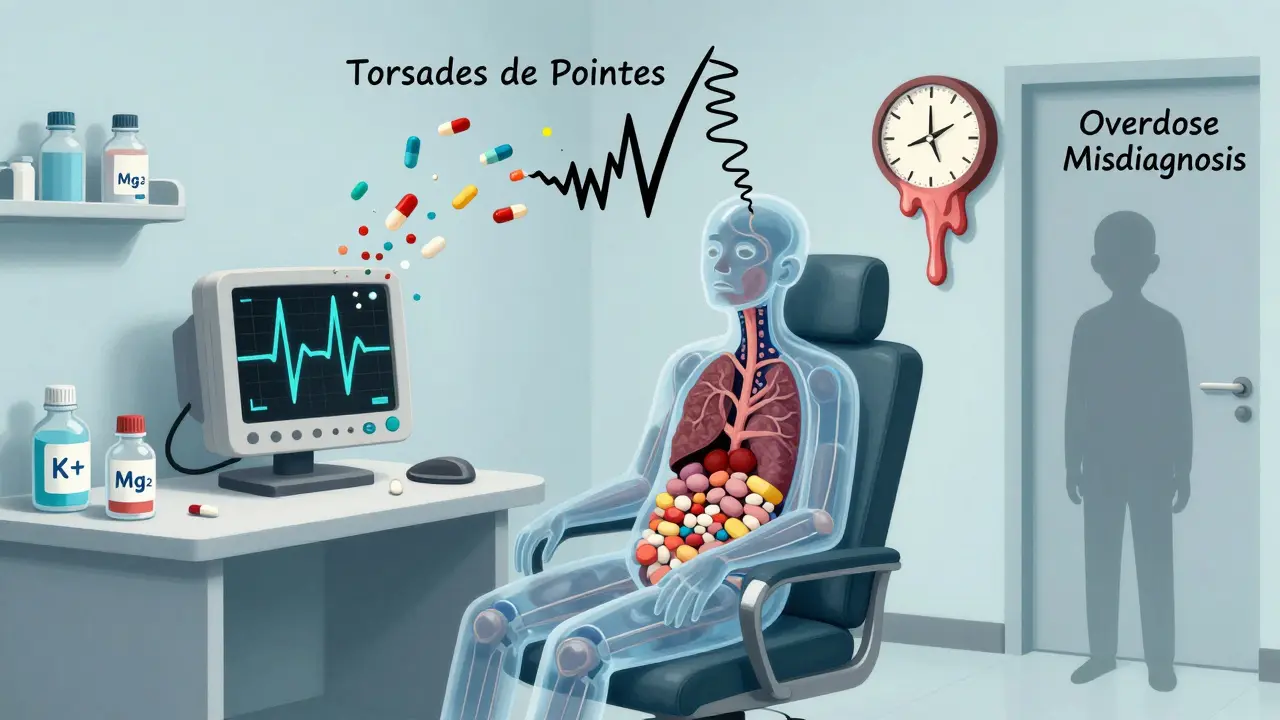
Methadone saves lives. For people recovering from opioid addiction, it reduces cravings, lowers the chance of overdose, and helps rebuild stability. But behind its benefits is a quiet danger: it can mess with your heart’s rhythm. Specifically, methadone can prolong the QT interval on an ECG-a measurement that shows how long your heart takes to recharge between beats. When this interval gets too long, it opens the door to a rare but deadly arrhythmia called Torsades de Pointes. This isn’t theoretical. Between 2000 and 2022, the FDA logged 142 confirmed cases of this arrhythmia linked to methadone. Many more likely went unreported because sudden death in someone on methadone is often written off as overdose, not cardiac arrest.
How Methadone Affects Your Heart
Methadone doesn’t just block opioid receptors. It also blocks a key ion channel in heart cells called hERG (KCNH2). This channel controls the flow of potassium out of the cell during the third phase of the cardiac action potential. When it’s blocked, the heart takes longer to reset, which shows up on an ECG as a longer QT interval. The effect is dose-dependent: higher doses mean more channel blockage. But it’s not always linear. Some people on low doses still develop significant prolongation, while others on high doses don’t. That’s why you can’t just rely on dose alone.
Other factors make it worse. Methadone can also slow your heart rate (bradycardia) and cause low magnesium or potassium levels. These changes compound the risk. If you’re on other drugs that also prolong QT-like certain antidepressants, antipsychotics, or antibiotics-the effect multiplies. Even something as simple as a fungal infection treated with fluconazole can spike methadone levels by 50%, pushing your QT interval into dangerous territory.
What’s a Normal QT Interval? And When Should You Worry?
Not all QT prolongation is the same. Doctors use a corrected version (QTc) to account for heart rate. Here’s the breakdown:
- Normal: ≤430 ms for men, ≤450 ms for women
- Borderline: 431-450 ms (men), 451-470 ms (women)
- Significantly prolonged: >450 ms (men), >470 ms (women)
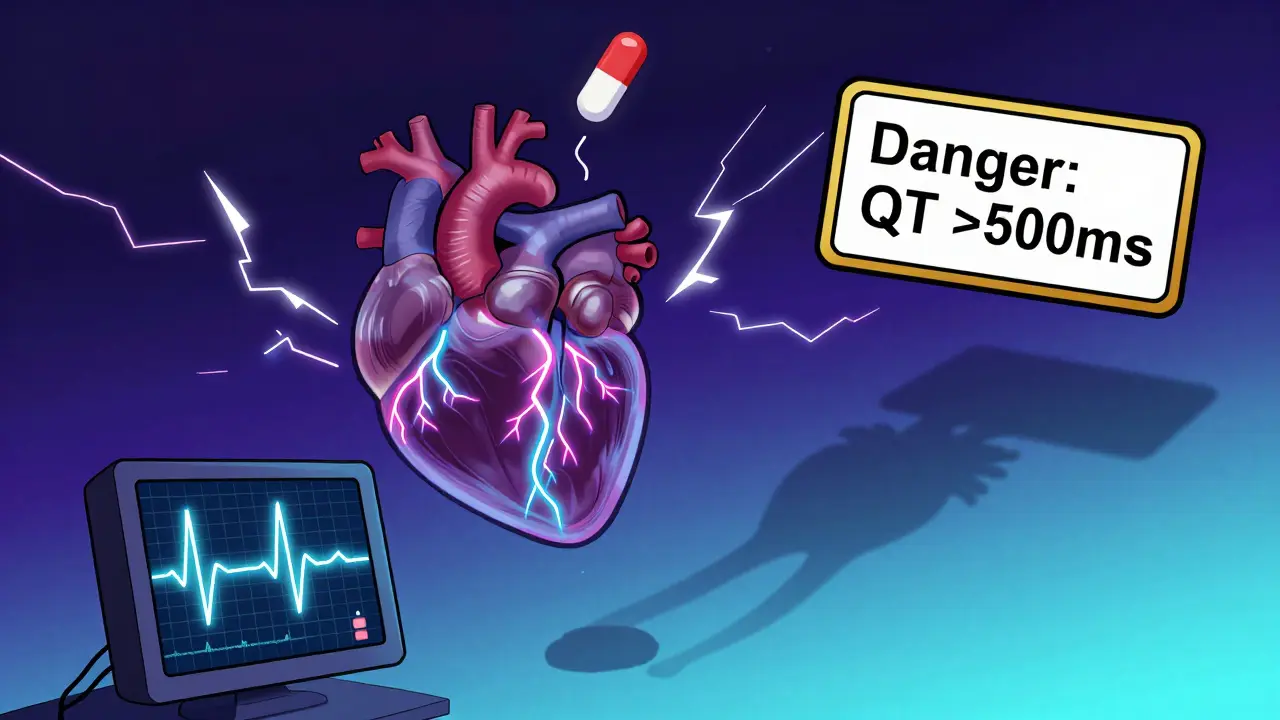
- Danger zone: >500 ms
At 500 ms or higher, your risk of sudden cardiac death jumps fourfold. Studies show that people with QTc >500 ms are far more likely to develop Torsades de Pointes. One 2017 study of 127 patients on methadone found that 8.7% had QTc over 500 ms. That’s nearly one in 10. And it wasn’t random-it was tied to high daily doses (>100 mg), low potassium, and taking other psychiatric meds.
Who’s at Highest Risk?
You can’t screen everyone the same way. Risk isn’t just about the dose-it’s about your whole picture. The biggest red flags:
- Female gender: Women have 2.5 times higher risk than men, even at the same dose.
- Age 65 or older: Older hearts handle electrical changes less well.
- Low potassium or magnesium: Levels below 3.5 mmol/L (potassium) or 1.5 mg/dL (magnesium) are dangerous.
- Slow heart rate: Under 50 beats per minute increases vulnerability.
- Heart disease: Heart failure, past heart attack, or reduced ejection fraction (<40%).
- Genetic risk: Congenital long QT syndrome-even if undiagnosed.
- Other QT-prolonging drugs: Tricyclic antidepressants, haloperidol, moxifloxacin, certain SSRIs.
- Drug interactions: Fluconazole, voriconazole, fluvoxamine, and even some HIV meds can double methadone levels.
If you have two or more of these, you’re already in the moderate-to-high risk group-even if your dose is under 100 mg/day.
When and How Often Should You Get an ECG?
Not everyone needs an ECG every week. But skipping it entirely is dangerous. Here’s what the guidelines say:
- Baseline ECG: Before starting methadone. This gives you a personal reference point.
- Follow-up ECG: At steady state-usually 2 to 4 weeks after starting or changing dose. Methadone builds up slowly in the body, and QT prolongation peaks around this time.
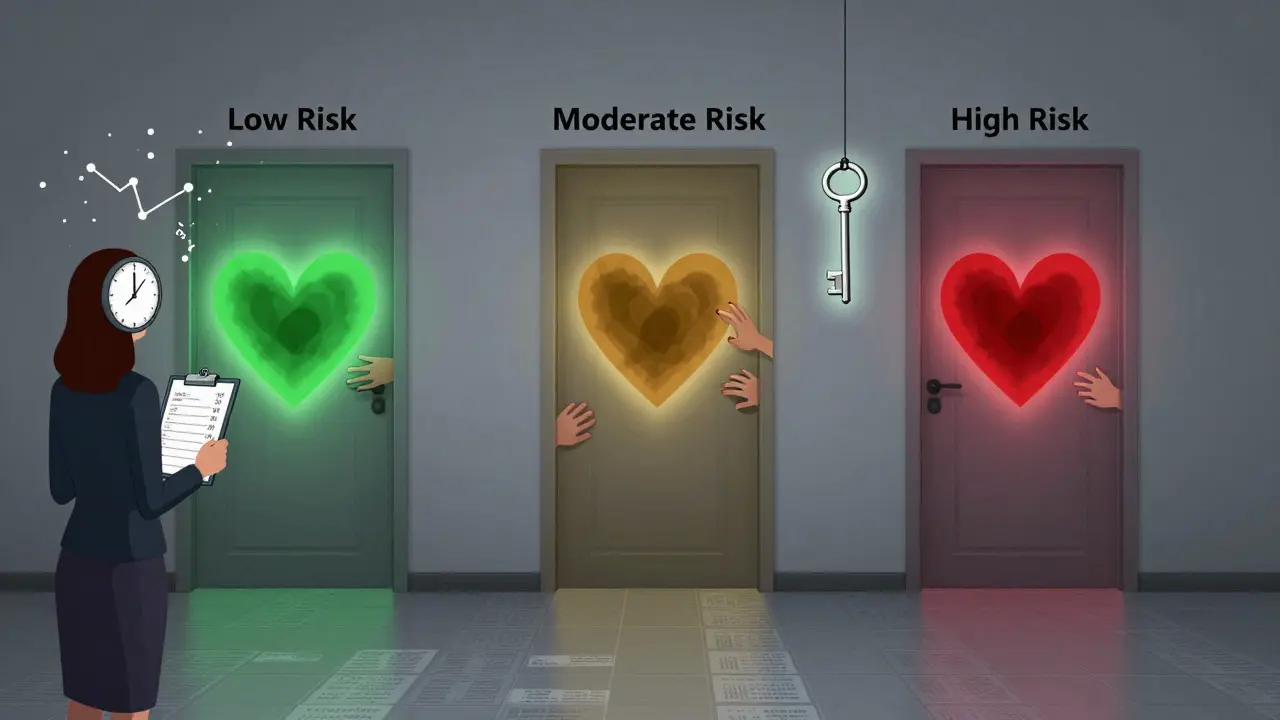
- Monitoring frequency: Based on your risk level:
| Risk Level | QTc Value | Additional Risk Factors | Monitoring Frequency |
|---|---|---|---|
| Low | <450 ms (men), <470 ms (women) | None | Every 6 months |
| Moderate | 450-480 ms (men), 470-500 ms (women) | 1-2 risk factors | Every 3 months |
| High | >480 ms (men), >500 ms (women) | 3 or more risk factors | Monthly |
If your QTc jumps more than 60 ms from baseline, or if it hits 500 ms or higher, you need immediate action: check electrolytes, consider lowering your dose, and get a cardiology consult. In many cases, switching to buprenorphine-a safer alternative with minimal QT effects-is the best next step.
Real-World Problems and Patient Experience
Here’s the ugly truth: not every methadone clinic follows these guidelines. A 2022 survey on Reddit (r/OpiatesRecovery) of 142 patients found that 68% reported inconsistent ECG monitoring. Some got regular tests. Others never had one. That inconsistency isn’t just frustrating-it’s life-threatening.
But those who did get regular monitoring? 82% said they felt safer. That’s not just confidence-it’s peace of mind. One patient wrote: “I didn’t know my QT was creeping up until my clinic finally did the test. My dose was 140 mg. My QTc was 490. They cut it to 100 and checked me monthly. I’m still alive.”
And it works. A 2023 study in JAMA Internal Medicine showed that clinics with structured QT monitoring cut serious cardiac events by 67%. That’s not a small win. That’s a life-saving protocol.
What You Can Do
If you’re on methadone:
- Ask for your baseline ECG. Don’t wait for them to offer it.
- Know your QTc number. Write it down. Ask for a copy of the report.
- Tell your prescriber about every other medication-even OTC ones, supplements, or herbal products.
- Get your potassium and magnesium checked regularly, especially if you have diarrhea, vomiting, or are on diuretics.
- If you feel dizzy, faint, or have palpitations, don’t brush it off. Get an ECG right away.
- If your clinic doesn’t monitor QT, ask why. Push for it. Your life depends on it.
If you’re a provider: Don’t assume low dose = low risk. Don’t skip ECGs because “they’re not in withdrawal.” Don’t blame sudden death on overdose without ruling out arrhythmia. Use the risk factors. Use the numbers. Use the guidelines.
What’s Next?
The science is clear: methadone is one of the most effective tools we have for opioid use disorder. But it’s not harmless. The risk of QT prolongation is real, predictable, and preventable. The question isn’t whether to monitor-it’s how to make sure everyone gets monitored. Every clinic, every provider, every patient. Because when you’re rebuilding your life, the last thing you should fear is your heart stopping.
Can methadone cause sudden death even if I’m not overdosing?
Yes. Methadone can trigger a deadly heart rhythm called Torsades de Pointes, which can lead to sudden cardiac arrest without any signs of overdose. This is especially true when QTc exceeds 500 ms. Many deaths in methadone patients are misclassified as overdose when they’re actually arrhythmias.
Do I need an ECG if I’m on a low dose of methadone?
Not always, but you still might need one. If you have other risk factors-like being female, over 65, on other QT-prolonging drugs, or have low potassium-you should get a baseline ECG even at low doses (e.g., 60-80 mg/day). Risk isn’t just about the dose-it’s about your whole health picture.
What if my QTc is borderline? Should I stop methadone?
No, you don’t need to stop. A borderline QTc (431-450 ms for men, 451-470 ms for women) doesn’t mean danger. But it does mean you need closer monitoring. Check your electrolytes, review all your meds, and repeat the ECG in 3 months. Many people stabilize or improve with simple adjustments.
Can I switch from methadone to buprenorphine if I’m worried about my heart?
Yes, and it’s often a smart move. Buprenorphine has minimal effect on the QT interval and carries far less cardiac risk than methadone. If you have multiple risk factors, a QTc over 480 ms, or a history of fainting or palpitations, switching should be seriously considered. Talk to your provider about a transition plan.
Why do some people on high methadone doses never have QT prolongation?
Genetics. Some people naturally have more resilient heart cells or better potassium regulation. Others may metabolize methadone faster due to genetic differences in liver enzymes (CYP3A4, CYP2B6). But you can’t assume you’re one of them. Without an ECG, you won’t know-and that’s why monitoring is non-negotiable.
How often should I get my potassium and magnesium checked?
At least every 3 months if you’re on methadone, especially if you’re in the moderate or high-risk group. If you have vomiting, diarrhea, heavy sweating, or take diuretics, check every month. Low electrolytes are one of the most easily fixed risk factors.
Can sleep apnea make methadone’s heart risks worse?
Yes. About half of people on methadone have sleep apnea. When you stop breathing during sleep, your oxygen drops, your heart rate fluctuates, and stress hormones spike-all of which can trigger arrhythmias. If you snore loudly, feel tired during the day, or have been told you stop breathing at night, get evaluated for sleep apnea. Treating it can reduce your cardiac risk.
Is there a safe upper limit for methadone dose?
There’s no absolute cutoff, but risk rises sharply above 100 mg/day. Studies show that patients on doses over 100 mg are over 3 times more likely to have QTc prolongation. Many experts recommend avoiding doses above 120-150 mg unless absolutely necessary and under close supervision. Always pair high doses with monthly ECGs and electrolyte checks.
Can I get an ECG at my regular doctor’s office, or do I need a specialist?
You can get a standard 12-lead ECG at most clinics, urgent cares, or hospitals. You don’t need a cardiologist for the test itself. But if your QTc is over 480 ms, or if it jumped more than 60 ms from baseline, you should see a cardiologist to evaluate whether your dose needs adjustment or if you need further testing like a Holter monitor.
What if my clinic refuses to do ECGs?
You have the right to your own health data. Ask for a written policy on QT monitoring. If they don’t have one, request a referral to a hospital or cardiology clinic for baseline testing. You can also ask your primary care provider to order the ECG. Your safety is non-negotiable. Don’t accept silence as an answer.

Comments (13)
Brandon Osborne
This is why I hate how clinics just hand out methadone like candy. No ECG? No labs? No monitoring? You're playing Russian roulette with someone's heart. I've seen guys drop dead and the clinic says 'overdose' because they don't want the liability. It's murder by bureaucracy.
Tatiana Barbosa
QT prolongation is real but often misunderstood. hERG blockade isn't the whole story-genetic polymorphisms in KCNH2 can make someone super sensitive even at 40mg. I've had patients with QTc 510ms on low doses and zero other meds. Screening isn't optional. It's basic harm reduction.
Ken Cooper
so wait… methadone blocks potassium channels? that’s wild. i thought it was just for the opioids. so like… if you’re on sertraline or ciprofloxacin? you’re basically stacking bombs? and women are more at risk? that makes sense tho. my cousin’s heart stopped and they blamed 'heroin overdose' but she was on methadone. no one checked her ekg. smh.
MANI V
This is what happens when you let drug addicts live. They get a free pass to poison their bodies while the system praises 'harm reduction.' No one talks about how methadone turns people into walking time bombs. The FDA data? That's just the tip. How many died quietly? How many families never got answers? This isn't medicine-it's a slow genocide.
Susan Kwan
Oh wow. A post that doesn't say 'methadone is safe' and actually tells you the risks? What is this, 2017? I'm crying. Someone finally wrote the truth instead of the opioid industry's PR pamphlet.
Random Guy
I took 120mg for 3 years. My QTc was 498. They told me 'it's fine.' I stopped cold turkey. Now I'm sober. And my ECG is normal. You don't need methadone to stay alive. You just need to stop being scared.
Ryan Vargas
Consider the epistemological framework here: if we define 'harm reduction' as the minimization of immediate mortality while ignoring the slow, systemic degradation of physiological integrity, are we not complicit in a form of structural violence? The hERG channel blockade is not merely pharmacological-it is a metaphysical rupture in the body's homeostatic covenant with the self. The fact that 8.7% of patients in that 2017 study exceeded 500ms isn't a statistic-it's a moral indictment of a healthcare system that prioritizes compliance over cardiac integrity.
John McDonald
Honestly, this is why I always tell my patients to get a baseline ECG before starting, then again at 30 days. And if they're on anything else that prolongs QT? Double-check electrolytes. Easy. Cheap. Could save a life. No one's asking for a cardiac MRI-just a $50 test. Why is that so hard?
Andy Cortez
they say 'methadone saves lives' but they never say 'methadone kills quietly.' i mean, if you get hit by a car, they know why you died. but if your heart just… stops… on methadone? 'oh, overdose.' like, no. no it's not. you're literally poisoning your own heart. and they call this treatment? this is just addiction with a medical label.
Joseph Charles Colin
The QTc threshold of 500ms is critical, but it's not absolute. The rate of torsades isn't linear-it's exponential beyond that point. Also, concomitant use of CYP3A4 inhibitors like fluconazole can elevate methadone plasma concentrations by up to 70%, not just 50%. The risk isn't just additive-it's multiplicative. Always check drug interactions. Always. Even if the patient says 'I only take one thing.'
Joshua Smith
I'm a nurse in an opioid treatment program. We do ECGs on everyone. We check K+ and Mg+ every month. We avoid fluconazole like the plague. It's not hard. It's just not always done. This info needs to be in every clinic. Not just big hospitals.
PAUL MCQUEEN
So we're supposed to monitor everyone? That's a nightmare. Who's gonna pay for all these ECGs? The system is already broke. Maybe we should just stop giving methadone to people who can't take care of themselves.
glenn mendoza
The ethical imperative to prioritize patient safety over institutional convenience cannot be overstated. The data presented herein, while clinically robust, underscores a profound failure in the implementation of evidence-based protocols within outpatient opioid treatment programs. It is not merely a pharmacological concern-it is a systemic failure of duty of care. I urge all stakeholders to institutionalize mandatory baseline and periodic ECG monitoring as a non-negotiable standard of practice.