Melanoma Risk Assessment Tool
Assess Your Risk Factors
Answer the following questions to calculate your personalized melanoma risk level.
Your Melanoma Risk Assessment
Spotting a problem early can be the difference between a quick treatment and a serious health battle. When it comes to skin cancer, knowing the subtle clues that hint at melanoma can save lives. Below you’ll find exactly what to watch for, how to check yourself, and when to get professional help.
Quick Takeaways
- Melanoma often starts as a mole that changes shape, color, or size.
- The ABCDE rule (Asymmetry, Border, Color, Diameter, Evolution) is a fast way to spot suspicious lesions.
- Heavy sun exposure, especially before age 30, dramatically raises risk.
- If you notice any change, schedule a dermatologist visit within two weeks.
- Early detection leads to a 99% five‑year survival rate, while late detection drops below 25%.
What Exactly Is Melanoma?
When talking about skin cancer, melanoma is the most aggressive form of skin cancer that originates in melanocytes, the cells that give skin its pigment. Unlike basal or squamous cell cancers, melanoma spreads quickly to lymph nodes and internal organs. Its danger lies in how fast it can move beyond the skin, making early identification crucial.
How Melanoma Fits Into the Bigger Picture of Skin Cancer
Skin cancer is an umbrella term for malignant growths arising from skin cells, including melanoma, basal cell carcinoma, and squamous cell carcinoma. While melanoma accounts for only about 1% of all skin cancers, it causes the majority of skin‑cancer deaths.
Common Early Signs to Watch For
Most melanomas begin as a mole or a spot that looks harmless at first. The key is to notice any deviation from its normal appearance. Here are the most frequent early indicators:
- New mole or spot after age 20.
- Change in an existing mole’s size, shape, or color.
- Irregular, uneven borders.
- Multiple colors in one lesion (brown, black, red, blue, or white).
- Diameter larger than a pencil eraser (about 6mm) - though melanomas can be smaller.
- Itching, tenderness, or bleeding without obvious cause.
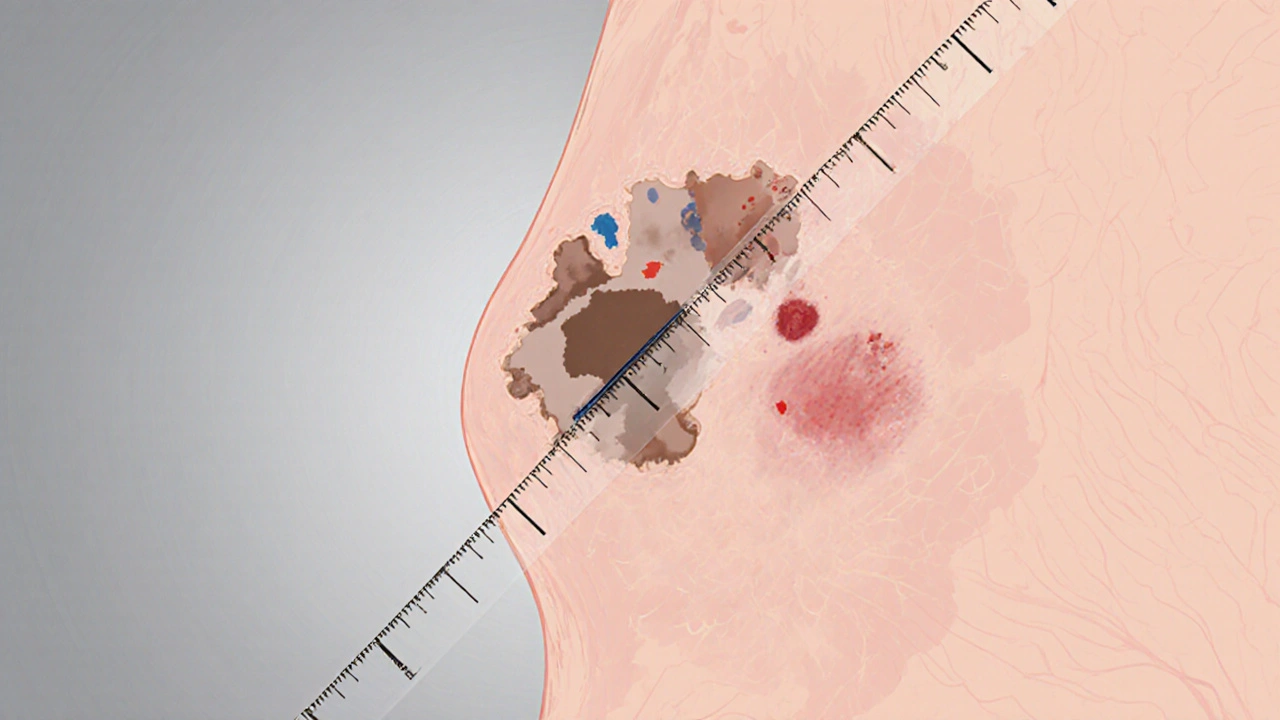
Using the ABCDE Rule for a Quick Self‑Check
The ABCDE rule gives a simple checklist you can run through in the mirror. It’s especially handy for busy people who don’t have time for a full dermatology textbook.
- Asymmetry: One half doesn’t match the other.
- Border: Edges are ragged, not smooth.
- Color: Varying shades in a single spot.
- Diameter: Bigger than 6mm (but remember, tiny lesions can still be melanoma).
- Evolution: Any change over weeks or months.
When you spot one or more red flags, treat it as a call to action.
Key Risk Factors You Can’t Ignore
Understanding what drives melanoma helps you gauge personal risk. Not all factors are within your control, but many are.
| Factor | Impact |
|---|---|
| Fair skin, red or blonde hair | Higher UV sensitivity, 2‑3× risk |
| History of sunburns (especially before age 30) | Significant increase in DNA damage |
| Excessive UV index exposure (UV‑B) | Directly damages melanocyte DNA |
| Family history of melanoma | Genetic predisposition, up to 10% of cases |
| Multiple or atypical moles (dysplastic nevi) | Each atypical mole adds ~2% risk per year |
| Immunosuppression (organ transplant, HIV) | Reduced immune surveillance, higher incidence |
While you can’t change your genetics, you can control sun behavior, wear protective clothing, and use sunscreen with at least SPF30.
When to See a Dermatologist
Self‑checks are a great first line, but a professional exam is the only way to confirm suspicion. Dermatologists are medical doctors specialized in skin, hair, and nail disorders, trained to perform skin examinations and biopsies. Schedule an appointment if you notice any of these triggers:
- Any new or changing spot that meets ABCDE criteria.
- Persistent itching, bleeding, or crusting.
- Family history of melanoma combined with a new mole.
- Unexplained skin changes after a severe sunburn.
Ideally, aim to see the dermatologist within two weeks of spotting the change.
How Diagnosis Works: From Biopsy to Pathology
If the dermatologist suspects melanoma, the next step is usually a biopsy performed by removing a small piece of the lesion for laboratory examination. Types of biopsies include:
- Excisional - whole lesion removed, gold standard for small moles.
- Punch - circular core taken, often for larger lesions.
- Incisional - part of a big lesion removed for assessment.
Pathologists evaluate the sample under a microscope, looking for the Breslow depth (tumor thickness) and ulceration status - factors that guide staging and treatment plans.

Self‑Exam Checklist: A Simple Routine
Make skin checks a habit. Here’s a step‑by‑step routine you can do once a month:
- Find a well‑lit room with a full‑length mirror and a hand‑held magnifying glass.
- Stand upright and scan the front of your body - face, neck, chest, arms, hands.
- Turn sideways, then look at the back of your body using a wall‑mounted mirror.
- Don’t forget less‑visible spots: scalp (use a comb), soles of feet, between toes, and genitals.
- Mark any mole that meets at least one ABCDE point on a skin‑tracking chart.
- Take photos of suspicious lesions for future comparison.
- Schedule a dermatologist visit if any listed changes appear.
Tracking changes over time is more reliable than trying to remember every mole’s look.
Preventive Measures: Sun Smart Habits
Prevention lowers the odds of a future melanoma. Follow these evidence‑backed habits:
- Apply broad‑spectrum SPF30+ sunscreen 15 minutes before going outdoors; reapply every two hours.
- Wear UPF‑rated clothing, wide‑brimmed hats, and UV‑blocking sunglasses.
- Seek shade between 10am and 4pm when UV index peaks.
- Avoid indoor tanning beds - they emit UV‑A that penetrates deep skin layers.
- Consider vitamin D supplementation if you limit sun exposure, after checking with a GP.
Even on cloudy days, UV rays can penetrate, so sunscreen isn’t just a summer habit.
Key Takeaways for Quick Reference
Copy this short list onto your phone notes or fridge:
- Watch for new or changing spots - think ABCDE.
- Do a full‑body self‑exam monthly.
- See a dermatologist within 2 weeks of any red flag.
- Protect skin daily with sunscreen and clothing.
- Know your personal risk (family history, skin type, sun habits).
Frequently Asked Questions
Can a mole be harmless and still meet the ABCDE criteria?
Yes. Some benign nevi show asymmetry or multiple colors, especially during puberty or pregnancy. However, any mole that meets two or more ABCDE points should still be evaluated by a dermatologist to rule out melanoma.
How often should I see a dermatologist if I have many moles?
People with numerous or atypical moles usually get a full skin check once a year. If any mole changes between visits, schedule an earlier appointment.
Is sunscreen enough to prevent melanoma?
Sunscreen is a vital part of protection, but combine it with shade, protective clothing, and UV‑avoidance during peak hours for the best defense.
What does a biopsy result look like?
The pathology report describes tumor thickness (Breslow depth in mm), ulceration status, mitotic rate, and whether cancer cells have reached deeper layers or lymph vessels. These details determine staging and treatment options.
Can melanoma appear on parts of the body not exposed to the sun?
Although sun‑exposed areas are most common, melanoma can develop on the soles of the feet, palms, under nails, and even the scalp under hair. Genetic factors play a larger role in those locations.


Comments (17)
Michelle Pellin
From the very first line, the guide drips with a theatrical flair that belies its clinical purpose.
The author paints the early signs of melanoma as if they were whispered secrets in a dimly lit salon, each mole described with a poetic eye.
Yet the practical steps are not lost; the checklist of skin type, mole count, and family history is crystal clear.
Readers can almost feel the urgency of early detection pulsing through the verses.
It is a rare blend of dramatics and precision that commands attention.
Keiber Marquez
This so-called guide pretends to be scientific while ignoring the real American sun exposure reality.
Lily Saeli
One could argue that the very notion of 'early signs' reflects a deeper philosophical battle between ignorance and enlightenment.
It is absurd that many still believe a single mole can be dismissed without contemplation.
The guide forces us to confront our complacency, demanding introspection about our skin's silent warnings.
In this way, it transcends mere medical advice.
Joshua Brown
First, understand that melanoma often masquerades as an ordinary freckle, which makes vigilance essential.
The guide’s risk assessment tool correctly emphasizes skin type; fair skin patients are at higher risk due to lower melanin protection.
Next, keep a log of any mole that changes in size, shape, or color-these are the hallmark warning signs.
Regular dermatology appointments, at least once a year, provide professional monitoring that self‑exams cannot replace.
Sunscreen with at least SPF 30 should be applied daily, even on cloudy days, to reduce UV damage.
Protective clothing and wide‑brimmed hats add another layer of defense.
If you notice the “ABCDE” criteria-Asymmetry, Border irregularity, Color variation, Diameter over 6 mm, Evolution-schedule an appointment immediately.
Finally, educate family members, because a shared awareness can lead to earlier detection across the household.
andrew bigdick
Totally agree, and I’d add that setting a monthly reminder on your phone can keep the self‑check habit consistent.
Also, many free apps let you photograph and track moles over time, which helps spot subtle changes.
Shelby Wright
Honestly, this whole moralizing tone about skin awareness feels like a melodramatic lecture; people already know the basics, they just need practical tools, not existential rants.
Ellen Laird
Ths guide is very informativ.
rafaat pronoy
Cool guide 😊; it’s straight‑forward and you can actually use the tool without a PhD.
sachin shinde
While the user‑friendly interface is commendable, the omission of precise statistical confidence intervals for the risk categories undermines the scientific rigor expected of such medical assessments.
Leon Wood
The excitement in this guide is palpable, and that energy can motivate anyone to take skin health seriously.
By breaking down the risk factors into bite‑size questions, the tool feels less intimidating.
It pushes readers to confront their sun‑light history without shame.
The vivid color cues for high, medium, and low risk instantly draw attention.
Moreover, the emphasis on early detection aligns perfectly with the latest oncology recommendations.
Keep spreading this enthusiasm, and more lives could be saved.
George Embaid
It's important to remember that skin tone diversity means risk manifests differently across cultures.
The guide wisely includes olive and brown skin categories, acknowledging the global audience.
Providing translations or culturally relevant examples would further broaden its reach.
Encouraging community workshops can also foster collective vigilance.
Let’s keep the conversation inclusive and supportive.
Meg Mackenzie
Some hidden agencies might be using these risk tools to track our sun habits for data mining, but still, the practical advice about checking moles is solid.
Shivaraj Karigoudar
The melanoma risk assessment platform amalgamates dermatological epidemiology with user-centric design, thereby facilitating a stratified risk perception among laypersons.
Leveraging a quintuple-factor algorithm-encompassing Fitzpatrick skin phototype, nevi count, hereditary predisposition, cumulative UV exposure before the third decade, and documented sunburn frequency-the system synthesizes a composite score that mirrors actuarial risk models employed in clinical settings.
Notably, the weighting schema allocates a higher coefficient to phenotypic attributes such as melanin paucity, reflecting the photoprotective correlation elucidated in peer‑reviewed literature.
Concurrently, the inclusion of behavioral variables acknowledges the modifiable nature of UV insults, thereby empowering preventive interventions.
The user interface presents a gradient color palette-emerald for low, amber for medium, and scarlet for high risk-anchored in established visual perception theory to expedite rapid comprehension.
Each selection field utilizes enumerated dropdown menus, reducing input ambiguity and standardizing data capture across heterogeneous user demographics.
Upon submission, the backend engine executes a deterministic calculation, eschewing stochastic variability to ensure reproducibility of the risk output.
The resultant risk tier is accompanied by a concise narrative synthesizing the “ABCDE” criteria, reinforcing heuristic vigilance.
Moreover, the platform furnishes evidence‑based recommendations, ranging from topical broad‑spectrum sunscreen application to referral pathways for dermoscopic examination.
Integration with electronic health record (EHR) APIs could further streamline clinical follow‑up, a feature poised for iterative development.
From a public health perspective, aggregating anonymized risk scores could inform geo‑spatial epidemiology, uncovering UV exposure hotspots and guiding resource allocation.
However, data privacy safeguards must be rigorously enforced to mitigate potential misuse of personal health information.
Future iterations might incorporate machine‑learning classifiers trained on longitudinal dermatoscopic image datasets, thereby enhancing predictive accuracy beyond static questionnaires.
In summation, the tool exemplifies a pragmatic convergence of biomedical insight and digital accessibility, positioning itself as a valuable adjunct in early melanoma detection strategies.
Stakeholders are encouraged to pilot the tool in community skin‑cancer screening programs to assess real‑world efficacy.
Matt Miller
Sounds solid; I’d love to see the pilot data.
Fabio Max
The collaborative spirit behind this guide is evident, and it shows how shared knowledge can demystify a scary disease.
Darrell Wardsteele
While the sentiment is commendable, the guide lacks rigorous citation of dermatologic studies, which weakens its credibility.
Madeline Leech
Anyone who skips this info is just asking for trouble.