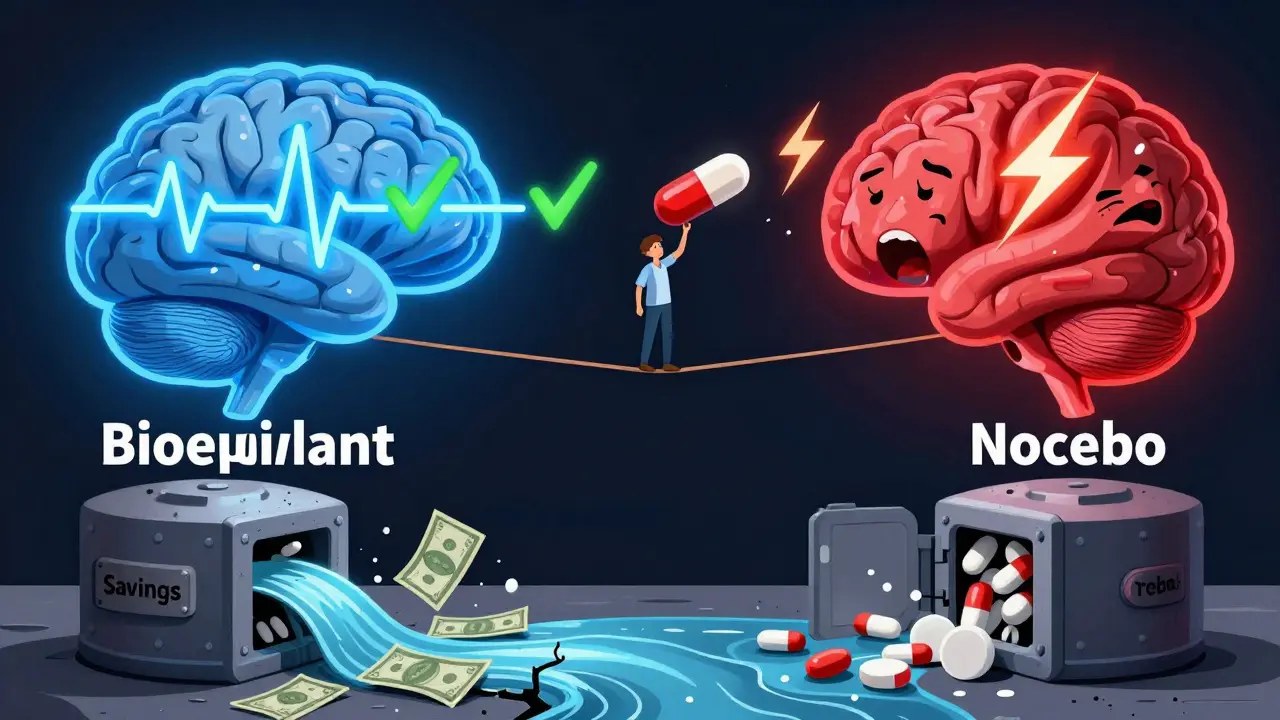
When you switch from a brand-name pill to a generic version, your body doesn’t change-but your mind might. You might feel like you’re getting less medicine. You might notice the pill looks different. You might start skipping doses. And suddenly, a simple cost-saving move turns into a health risk.
More than 90% of prescriptions in the U.S. are filled with generic drugs. They’re cheaper, FDA-approved, and chemically identical to their brand-name counterparts. But despite all that, medication adherence drops by an average of 15% after the switch. That’s not because generics don’t work. It’s because people think they don’t.
Why Patients Stop Taking Their Generic Medications
The science is clear: generic drugs must meet the same strict standards as brand-name drugs. They contain the same active ingredient, in the same strength, and work the same way in the body. The FDA requires them to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream within an acceptable range.
So why do so many people stop taking them?
It’s not about chemistry. It’s about perception.
A 2018 study showed patients given placebo pills labeled as "generic" reported more pain and took more extra pills than those given the exact same placebo labeled as "brand-name." The pills were identical. The only difference was the label. That’s the nocebo effect in action-when negative expectations make you feel worse.
Other reasons patients discontinue generics:
- The pill looks different-smaller, different color, no logo
- They remember a friend who "had bad side effects" after switching
- They assume cheaper means lower quality
- They’re confused by multiple generic versions from different manufacturers
A University of Michigan study found that nearly 3 in 10 elderly patients got confused when their pill changed shape or color. For someone taking five or more meds a day, that’s enough to make them skip a dose-or worse, take the wrong one.
Where the Switch Goes Wrong: High-Risk Medications
Not all drugs are created equal when it comes to switching. Some medications leave little room for error.
Narrow therapeutic index (NTI) drugs are one example. These are medicines where even tiny changes in blood levels can cause serious problems. Think:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Lamotrigine (seizure medication)
- Phenytoin (anti-seizure)
A 2017 NEJM study found patients switched to generic versions of these drugs had a 0.8% higher chance of being hospitalized. That might sound small-but in a population of millions, it adds up to thousands of avoidable hospital stays.
And then there’s mental health. A 2020 study in CNS Drugs showed antidepressant discontinuation rates jumped 19.4% after switching to generics. Why? Because patients with depression are especially sensitive to changes in how they feel. Even if the drug works the same, if they think it’s "not working," they’re more likely to quit.
On the flip side, statins (cholesterol drugs) actually saw better adherence after switching to generics. Why? Because the copay dropped from $50 to $5. For many people, cost is the biggest barrier to taking medicine daily. When that barrier disappears, they take it.
The Hidden Culprit: Inactive Ingredients
Generics aren’t just the active ingredient. They also contain fillers, dyes, and binders-the "inactive" parts. These don’t treat your condition. But they can cause problems.
A 2021 JAMA Dermatology study found that 3.7% of patients had allergic reactions to dyes or fillers in generic pills. That’s rare-but it’s real. One patient might get a rash from a red dye in a generic version of their blood pressure pill. The brand-name version used a different dye. The active ingredient? Same. But the reaction? Real.
And for people with food allergies or sensitivities (like gluten or lactose), those inactive ingredients matter. Some generics contain lactose as a filler. If you’re lactose intolerant, you might feel bloated or nauseous-not because the medicine isn’t working, but because your body is reacting to the filler.
That’s why it’s important to check the pill’s ingredients. Not all pharmacists do this automatically. But if you’ve had a reaction before, ask: "Is this the same filler as before?"

What Providers and Pharmacists Should Do
Switching to a generic isn’t just a pharmacy transaction. It’s a clinical decision.
Yet a 2022 audit found that only 28% of patients were told the generic was bioequivalent. Only 19% were asked if they had concerns.
Here’s what works:
- Explain bioequivalence clearly. Don’t say, "It’s the same." Say, "This generic has been tested to deliver the same amount of medicine into your bloodstream as the brand. The FDA requires it. It’s not a cheaper version-it’s an equal version."
- Describe the physical differences. "The brand was blue and round. This one is white and oval. The medicine inside is the same."
- Highlight the cost savings. "This switch will cut your monthly cost from $80 to $10. That’s $840 saved a year."
- Ask for concerns. "Have you ever had a bad experience with a generic before? Are you worried this one won’t work?"
- Follow up. A 2022 meta-analysis found that patients who got a phone call from their pharmacist within 72 hours of switching were 31% more likely to keep taking their meds.
Don’t assume patients understand. A 2021 study showed 47% of patients with low health literacy thought "generic" meant "weaker."
What Patients Can Do to Stay on Track
You don’t have to wait for your provider to explain everything. You can take control.
- Keep a pill log. Write down what you take, when, and how you feel. If you notice a change after switching, you’ll have data to share with your doctor.
- Use a pill organizer. If the shape or color changes, a weekly organizer with labeled slots prevents mix-ups.
- Ask for the same manufacturer. If you did well on one generic, ask if you can stick with the same brand of generic. Some manufacturers make more consistent versions.
- Check the label. Look up the inactive ingredients on Drugs.com or the FDA website if you have allergies.
- Don’t assume it’s broken. If you feel different after switching, don’t stop. Call your pharmacist. It might be your body adjusting-or it might be a nocebo effect.
One patient on Reddit shared: "I stopped my generic blood pressure pill because I felt dizzy. I called my pharmacist. They said the new version had a different filler. I switched back to the old generic-and my dizziness went away. Now I always ask for the same one."
Technology Is Helping-But It’s Not Enough
New tools are making adherence easier.
Surescripts’ e-prescribing system now flags brand-to-generic switches so pharmacists know to counsel the patient. Medication synchronization programs-where all your refills are due on the same day-boost adherence by 18% for generic users.
And then there’s AI. A 2023 study tested an app called AiCure that uses your phone’s camera to watch you swallow your pill. It sent reminders and tracked adherence. For patients switching to generics, it improved compliance by 37%.
But tech alone won’t fix this. The real solution is human connection.
The Bigger Picture: Why This Matters
Medication non-adherence costs the U.S. healthcare system $528 billion a year. That’s more than heart disease or diabetes. And a big chunk of that comes from patients stopping their meds after switching to generics.
Generics save money-$132.7 billion in 2023 alone. But if patients stop taking them, those savings vanish. Hospitals get busier. ER visits go up. Complications grow.
The FDA’s 2023 Generic Drug Communication Initiative will require manufacturers to include transition guides with every new generic. Starting in 2025, you’ll get a sheet explaining: "This is the same medicine. Here’s why it looks different. Here’s what to do if you’re worried."
And the Generic Pharmaceutical Association is launching a "Seamless Switch" certification. Drugs that keep the same shape, color, and size during brand-to-generic transitions will get a special label. That’s huge for elderly patients who rely on visual cues.
For now, the best tool you have is knowledge. And the best person to give it to you? Your pharmacist.
Final Thought: It’s Not About the Pill. It’s About the Trust.
A generic drug isn’t a downgrade. It’s a smart choice. But trust doesn’t come from a label. It comes from conversation.
If you’ve ever felt like you got "less" medicine after a switch-you’re not alone. But you’re not wrong to care. Your body is listening. So is your mind.
Ask questions. Speak up. Use tools. Stay on track. And remember: the medicine in that pill? It’s the same. You just need to believe it.


Comments (10)
Arjun Seth
People are so weak nowadays. You switch pills and suddenly your mind starts playing tricks on you? Grow up. If you can't handle a different-shaped pill, maybe you shouldn't be taking medicine at all. The FDA doesn't lie. Your body doesn't care what color it is. Stop making excuses.
Ayush Pareek
I get it. Switching generics can feel weird, especially if you've been on the same brand for years. But you're not alone. I switched my blood pressure med last year and felt the same way-until I tracked my numbers. Same readings. Same energy. The pill just looked different. Give it time. Your body knows what it's doing.
Jami Reynolds
Let me be clear: this isn't about perception. It's about corporate manipulation. The FDA is influenced by Big Pharma. Generic manufacturers cut corners. The bioequivalence standards? A joke. I've seen patients crash after switching-kidney failure, arrhythmias, seizures. They call it 'nocebo.' I call it cover-up. They don't test long-term. They don't test real-world interactions. And now they want you to trust a white oval pill with no logo? Please.
Frank Geurts
As someone who has lived in six countries and observed healthcare systems across continents, I can attest that the American fixation on pill aesthetics is uniquely cultural. In Japan, patients receive generic medications with formal printed guides and ceremonial packaging. In Germany, pharmacists conduct mandatory counseling. Here? We hand you a pill in a plastic bag and say, 'It's the same.' No wonder trust evaporates. This is not a medical issue-it is a communication failure rooted in systemic neglect.
Dan Mack
They're lying to you. The generics aren't the same. The FDA lets them be 20% off in absorption. That's not bioequivalent-that's a gamble. My cousin died after switching to generic levothyroxine. They said it was 'coincidence.' Coincidence my ass. They don't want you to know this. They want you to save $5 so they can keep raising prices on the brand. Wake up.
Amy Vickberg
My dad switched to generic statins and started taking them again after years of skipping because the copay dropped from $75 to $8. He said he felt better, not worse. I think the problem isn't the pill-it's the story we tell ourselves about it. When we assume the cheap one is worse, we make it true. Change the story. Change the outcome.
Nishant Garg
Let me tell you something about India-we’ve been using generics for decades. In rural clinics, people get the same medicine in different colors every month. No one panics. Why? Because they’re not told it’s 'different.' They’re told it’s 'the same medicine, cheaper.' No drama. No labels. Just results. Here, we treat medicine like a luxury product with branding. In the real world, it’s just chemistry. Maybe we need to stop overthinking it and start trusting science.
Nicholas Urmaza
Stop treating patients like children. If you can't handle a pill change, you're not ready for responsibility. The system is designed to save money and lives. Stop blaming generics. Start taking your meds. Your health isn't a Netflix subscription-you don't get to pick the packaging. Take the pill. Period.
Sarah Mailloux
I used to be the person who stopped taking generics because they looked weird. Then I started using a pill organizer with labels. Now I don’t even notice the difference. It’s not about the pill-it’s about the habit. Find your system. And if you’re worried? Call your pharmacist. They’re not just there to hand out pills. They’re there to help.
Nilesh Khedekar
Oh wow. A 37% improvement with an app that watches you swallow your pill? That’s not innovation. That’s surveillance. Next they’ll put microchips in the pills and bill you for the data. Meanwhile, the real solution? Stop switching generics unless you’re forced to. And if you are? Demand the same manufacturer. Don’t let the pharmacy play roulette with your thyroid. I’ve seen too many people get sick because someone else decided to save a dollar.