Most people will experience low back pain at some point in their life. It’s not rare-it’s normal. But when that pain sticks around, gets worse, or comes with strange symptoms, it’s easy to panic. Is it just a pulled muscle? Or could something serious be going on? The truth is, low back pain is almost always harmless. But knowing when it’s not-that’s what saves people from permanent damage and unnecessary scans.
Red Flags: What Actually Matters
You’ve heard the term "red flags" before. Maybe your doctor mentioned it, or you saw it online. But not all red flags are created equal. Out of the 46 different signs doctors have listed over the years, only a handful actually mean something serious.Let’s cut through the noise. The real red flags-those that need immediate attention-are tied to four dangerous conditions: cancer, broken bones, infection, and cauda equina syndrome.
For cancer, the clearest warning signs are a history of cancer (especially breast, lung, or prostate) and unexplained weight loss-like dropping 10 pounds in a few months without trying. If you’ve had cancer before and now your back hurts, don’t wait. Same goes for someone on long-term steroids or with a weakened immune system. These aren’t just "maybe" signs-they’re strong indicators.
Fractures? Think trauma. A fall from height, a car crash, or even a simple stumble if you’re over 65 and have osteoporosis. If you’re on bone-thinning meds like prednisone and your back suddenly hurts after a minor bump, get checked. The sensitivity isn’t perfect, but the specificity is high. That means when it’s there, it’s usually real.
Now, the big one: cauda equina syndrome. This is rare-but devastating if missed. It happens when nerves at the bottom of your spine get crushed. The signs are unmistakable: you can’t control your bladder or bowels, you feel numbness in your saddle area (that’s the part that touches a bike seat), or you can’t feel your anal sphincter when the doctor checks. If you have urinary retention with more than 200cc left in your bladder after peeing, plus saddle numbness, your chance of having this is over 90%. This isn’t "wait and see" territory. You need an MRI within hours. Surgery within 48 hours gives you the best shot at avoiding permanent nerve damage.
And what about night pain? Or fever? These get thrown around a lot. Night pain can be a red flag, but it’s also common in people with just a stiff back. Fever? Sure, it could mean infection. But most people with low back pain and a low-grade fever have a virus-not spinal osteomyelitis. Don’t panic over these alone. They need to show up with other signs.
Imaging: When It Helps, When It Hurts
You’ve probably seen someone get an X-ray or MRI for back pain. Maybe you’ve had one yourself. But here’s the hard truth: for 97% of people with low back pain, imaging doesn’t help. It doesn’t speed up recovery. It doesn’t reduce pain. And it often makes things worse.Why? Because scans show things that aren’t the problem. Bulging discs? Herniations? Degeneration? These are normal in people with zero pain. In fact, up to 40% of healthy 30-year-olds have disc bulges on MRI. Finding one doesn’t mean it’s causing your pain. But once you see it, your brain starts linking pain to that image-and suddenly, you’re scared to move, you avoid activity, and your recovery slows down.
Guidelines from the American College of Radiology, the Canadian Family Physicians Association, and the American Academy of Family Physicians all agree: if you have low back pain for less than 4 weeks and no red flags, don’t get imaging. Not an X-ray. Not an MRI. Nothing.
When is imaging appropriate? Only if red flags are present. For suspected cancer or nerve compression, MRI without contrast is the gold standard. For infection, a bone scan with SPECT/CT or a contrast-enhanced CT is better. X-rays? They’re almost useless unless you’ve had trauma or are over 70 with suspected fracture. Even then, they don’t show soft tissue damage. A negative X-ray doesn’t rule out a serious problem.
And here’s the kicker: a 2022 survey found that nearly half of primary care doctors still order X-rays for acute back pain without red flags. Why? Time pressure. Fear of missing something. Patient demand. But the cost isn’t just financial-it’s psychological. People who get early scans are more likely to develop chronic pain, take more opioids, and have more surgeries down the line.
Exercise Therapy: The Only Treatment That Works Long-Term
If not imaging, then what? The answer is simple: movement.Exercise therapy isn’t just "good for you." It’s the most effective treatment for low back pain that we have. A Cochrane Review of 97 studies with nearly 20,000 people found that those who exercised had significantly less pain and better function than those who did nothing. The improvements lasted for months-even years.
Not all exercises are equal. Motor control exercises-like learning to engage your deep core muscles without gripping your glutes or holding your breath-have the strongest evidence. Graded activity, where you slowly increase your activity level even if you’re in pain, works well too. And combined programs-mixing strength, aerobic work, and flexibility-are the most practical for most people.
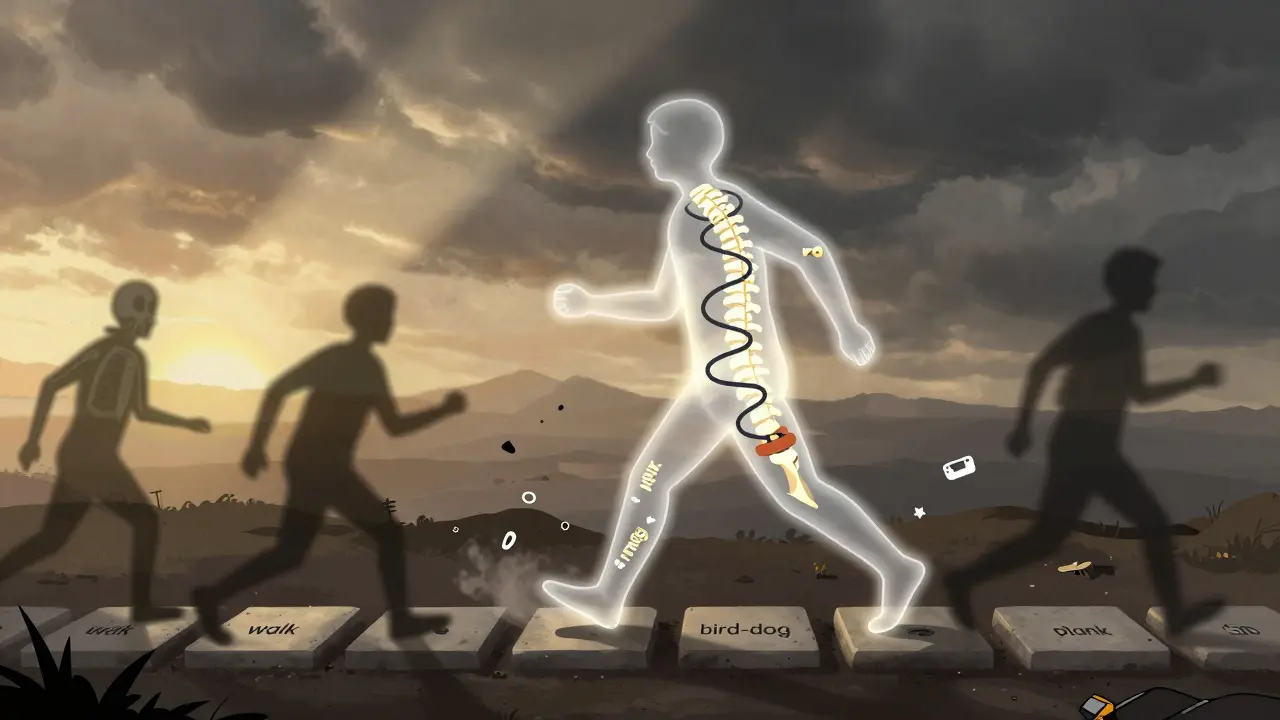
Here’s what a real exercise plan looks like:
- Start with 2-3 supervised sessions per week for 4-6 weeks. A physiotherapist will teach you how to move safely.
- Focus on control, not intensity. Don’t try to lift heavy right away. Learn to stabilize your spine first.
- Progress gradually. After 4-6 weeks, increase strength work to 70-85% of your one-rep max. Add walking or cycling for 20-30 minutes, 3-5 days a week.
- Transition to a home program. You don’t need a gym. Bodyweight squats, bridges, bird-dogs, and planks work just fine.
Adherence is everything. If you stop after two weeks, you get no benefit. Studies show that people who stick with exercise for 8-12 weeks cut their risk of future episodes by nearly 50%.
And here’s something most people don’t realize: you don’t need to be pain-free to start moving. In fact, moving while you’re sore is often the key to breaking the cycle. Pain doesn’t equal damage. It’s your nervous system being overly protective. Exercise retrains it.

What Doesn’t Work (And Why You Should Avoid It)
There’s a lot of noise out there. Back braces. Spinal adjustments. TENS machines. Ultrasound. Injections. Some work for short-term relief. None change the long-term outcome.Braces? They make your muscles weaker. You become dependent on them. The evidence? Weak at best.
Chiropractic adjustments? They might feel good for a day or two. But they don’t reduce pain more than exercise or education. And if you have red flags, adjustments can be dangerous.
Spinal injections? Cortisone shots might temporarily reduce inflammation, but they don’t fix the root cause. And repeated shots can damage tissue over time.
And please, don’t rely on age as a red flag. Being over 50 or 55 doesn’t mean you have cancer or a fracture. That myth is still floating around clinics. A 2023 update to the UK’s NICE guidelines removed age over 55 as a red flag-because the data shows it doesn’t predict serious disease.
What You Can Do Today
If you have low back pain, here’s your action plan:- Stay active. Don’t rest. Walk. Move. Even if it’s slow.
- Look for red flags: unexplained weight loss, history of cancer, loss of bladder/bowel control, saddle numbness, or trauma. If any of these are present, go to urgent care or the ER.
- Don’t demand imaging. Ask your doctor: "Is there a red flag?" If not, ask: "Can I start moving?"
- Find a physiotherapist who specializes in back pain. Not one who pushes needles or machines. One who teaches you how to move better.
- Commit to 8-12 weeks of exercise. Even 15 minutes a day. Consistency beats intensity.
Low back pain is frustrating. It’s expensive. It’s misunderstood. But it doesn’t have to be a life sentence. Most people recover fully-not because of a scan, not because of a shot, but because they got moving, learned how to protect their back, and stopped fearing their own body.
Are red flags always accurate for detecting serious back problems?
No. Most red flags have low sensitivity, meaning they often miss serious conditions. But they have high specificity-so when they’re present, the risk is real. The biggest problem isn’t missing red flags-it’s overreacting to them. Many people get scanned because of vague symptoms like night pain or age, even when the chance of cancer or infection is less than 1%. That’s why guidelines now stress using red flags as part of a bigger picture, not as standalone triggers.
Can I still exercise if my back hurts?
Yes-and you should. Pain during movement doesn’t mean you’re damaging your spine. Most back pain is due to sensitivity in the nervous system, not tissue damage. Gentle movement helps calm that system. Start with walking, pelvic tilts, or cat-cow stretches. Avoid positions that cause sharp pain, but don’t stop moving because of dull or achy discomfort. The goal is to gradually increase your tolerance, not to be pain-free before you start.
Why do doctors still order X-rays for back pain if guidelines say not to?
Time pressure, fear of lawsuits, and patient expectations. Most doctors spend less than 13 minutes per back pain visit-far less than the 18-22 minutes needed to properly assess red flags and explain why imaging isn’t needed. Many patients expect a scan, and doctors sometimes give in to avoid conflict. But studies show that when doctors explain the evidence clearly, most patients are happy to avoid unnecessary tests.
Is MRI always better than X-ray for back pain?
Only if you have red flags or neurological symptoms. For routine low back pain, MRI doesn’t help-and can hurt by showing harmless changes that lead to fear and inactivity. X-rays are better for detecting fractures after trauma, but even then, they miss soft tissue injuries. MRI is the best tool for nerve compression, infection, or tumors-but only when there’s clinical suspicion. Don’t assume MRI = better. It’s only better when used correctly.
How long does it take for exercise therapy to work for low back pain?
Most people start feeling better in 2-4 weeks, but real change takes 8-12 weeks. Pain reduction and improved function show up slowly because you’re retraining your nervous system and strengthening deep muscles that have been inactive for months or years. The key isn’t speed-it’s consistency. People who do exercises 3 times a week for at least two months cut their risk of future pain by nearly half. Skipping sessions or quitting early means you won’t get lasting results.


Comments (12)
lisa Bajram
Okay but let’s be real-most people don’t have access to a physio who actually knows what they’re doing. I got handed a PDF and told to ‘do bridges’ and now my glutes scream at me every morning. Where do you even find one of these magic therapists? And why do they cost more than my rent?
anthony martinez
Doctors order X-rays because patients scream until they get one. It’s not malpractice-it’s emotional triage. You don’t fix a system by shaming the people stuck in it.
neeraj maor
They’re lying. MRI’s don’t show nerve compression? Then why do half the spine surgeons I’ve met swear by them? This is Big Pharma’s cover-up. They don’t want you moving-you need their $12,000 injections and 18-session rehab packages. Wake up.
Dwayne Dickson
While I appreciate the evidence-based framework presented herein, one must interrogate the underlying epistemological assumptions regarding the biopsychosocial model’s applicability in primary care settings where temporal constraints are non-negotiable. The assertion that ‘pain does not equal damage’ is theoretically sound, yet empirically insufficient when contextualized within the phenomenological experience of chronic discomfort.
Mario Bros
Just started walking 15 mins a day after reading this. My back hasn’t felt this good in 3 years. No scans. No pills. Just me, my sneakers, and a stubborn refusal to quit. You got this.
Ashlee Montgomery
What if your nervous system is scared because your body has been betrayed before? What if the pain isn’t about tissue but about memory? Maybe movement isn’t the cure-it’s the conversation.
Kunal Majumder
Bro I was skeptical too but I did bird-dogs every morning for 6 weeks. Now I can pick up my kid without wincing. No fancy gear. Just consistency. You don’t need a gym. Just show up.
Ritwik Bose
🙏 Thank you for this. I’m from India and here, everyone assumes back pain = ‘disc problem’ and rushes to get an MRI. I showed my doctor this and he actually listened. No scan. Just exercises. It’s working. 🙏
Paul Bear
Correction: The 2023 NICE guidelines didn’t remove age over 55 as a red flag-they clarified that age alone is not a predictive factor. Your phrasing implies a misinterpretation of the evidence. Please cite properly before making sweeping claims.
Jaqueline santos bau
So you’re saying I should just ‘move through it’ after my husband left me, my mom died, and my job fired me? Like my back pain is just… a vibe? Maybe I’m not the one who needs to ‘stop fearing my body’-maybe the system that ignores trauma needs to stop gaslighting people.
Jake Nunez
My physical therapist told me the same thing. Said my MRI showed ‘normal aging’-which, by the way, is just another way of saying ‘your body is a human being, not a broken machine.’
Jake Kelly
Thank you for writing this. I’ve been telling my friends for years: stop Googling your pain. Start moving. It’s not magic. It’s medicine.