Imagine taking a pill that’s chemically identical to your usual medication-same active ingredient, same dose, same manufacturer-but now it’s in a plain white bottle labeled generic. You’ve been told it’s just as good. But do you really believe it? What if, without knowing why, you start feeling worse? More side effects. Less relief. Maybe you even stop taking it altogether.
This isn’t imagination. It’s real. And it’s called the labeling effect.
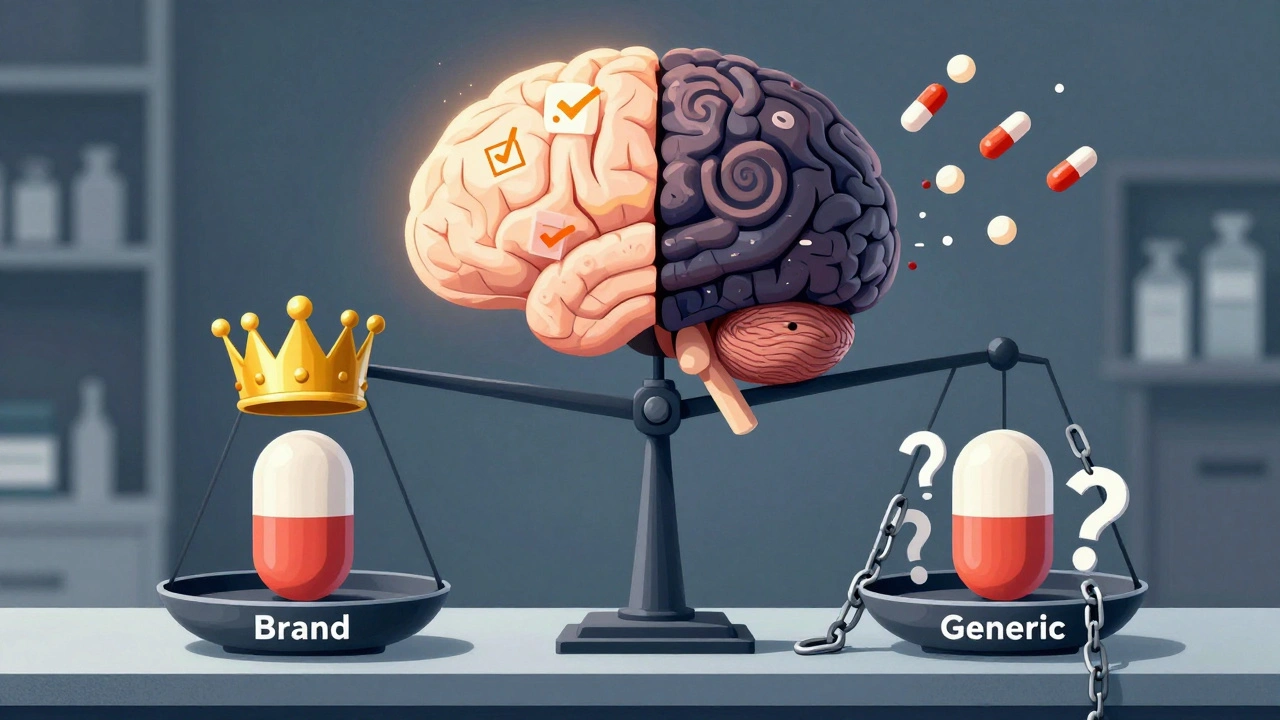
For decades, doctors and pharmacists have assumed that if two drugs have the same active ingredient, they work the same way. And scientifically, they’re right. But biology isn’t the whole story. The mind plays a powerful role-and the label on the bottle can change how your body responds.
What Exactly Is the Labeling Effect?
The labeling effect is the phenomenon where the name or branding on a medication changes how patients experience it-even when the drug is identical. A pill labeled "generic" can feel less effective, cause more side effects, and lead to higher discontinuation rates than the exact same pill labeled as a brand-name drug.
This isn’t about quality. It’s about perception. And it’s backed by solid science.
In a 2019 study published in the European Journal of Public Health, researchers gave 72 participants identical placebo pills. Half were told they were taking a brand-name drug. The other half were told they were taking a generic version. After just seven days, 54% of those who believed they were taking the generic drug stopped taking it. Only 33% of the brand-name group did. That’s a 21-percentage-point drop in adherence-just because of a label.
And it wasn’t just about quitting. People in the generic group reported higher pain levels, more side effects, and even took extra pills from other bottles to "make up" for what they thought was a weak medication.
Placebo Power: How a Fake Pill Can Work Better With a Brand Name
One of the most striking findings came from a 2016 study led by Dr. Keith Petrie at the University of Auckland. Researchers gave 87 students either real ibuprofen or a sugar pill-both labeled either as a brand-name drug or as generic.
The results? The brand-name placebo (a sugar pill labeled as a brand) reduced pain almost as well as the real ibuprofen. The generic placebo? Not even close.
Patients who thought they were taking a brand-name placebo reported a pain reduction of 3.0 cm on a 10-cm scale. Those who thought they were taking a generic placebo? Only 1.8 cm. That’s a 40% drop in perceived effectiveness-just because of the label.
And here’s the kicker: 63% of people said the brand-name placebo relieved their headache. Only 42% said the same about the generic placebo-even though both were sugar pills.
This isn’t magic. It’s the placebo effect in action. But here’s the twist: the placebo effect doesn’t work equally for everyone. Brand names trigger trust. Generic labels trigger doubt.
Why Do People Trust Brand Names More?
It’s not irrational. It’s learned.
Brand-name drugs come with advertising, recognizable logos, packaging, and years of marketing that say: "This works. This is reliable. This is trusted." Generic drugs? Often come in plain packaging. No ads. No name recognition. Just a chemical name and a price tag.
People associate brand names with quality-even when they know better. A 2023 Kaiser Family Foundation survey found only 56% of Americans believe generic drugs are "as good as" brand-name drugs. That’s down from 62% in 2018. And this gap isn’t shrinking.
It’s worse for older adults and those with lower health literacy. In the 2019 study, patients with low health literacy were nearly twice as likely to stop taking a generic-labeled pill than those with high health literacy. They didn’t question the science. They trusted the label.
And it’s not just patients. Pharmacists and doctors report the same thing. A 2022 survey by the American Pharmacists Association found that 63% of pharmacists had been asked by patients or doctors: "Is this generic really the same?"
The Dark Side: When Labels Cause Real Harm
The labeling effect isn’t just about discomfort. It can lead to real health risks.
When patients stop taking their medication because they think it’s "not working," their condition worsens. For someone with high blood pressure, diabetes, or epilepsy, skipping doses isn’t a minor inconvenience-it’s dangerous.
Worse, some generic labels don’t match the original brand’s wording. A 2020 study analyzed 31 drug products and found that every single one had differences between the brand and generic labeling. In 12.9% of cases, those differences could cause life-threatening errors. In 35.5%, they could cause serious harm.
For example, a generic version might say "take with food" while the brand says "take on empty stomach." Or it might leave out a warning about interactions with alcohol. These aren’t mistakes-they’re gaps in regulation.
The FDA requires generics to match the brand’s active ingredient. But inactive ingredients? Formatting? Warnings? Those can vary. And patients don’t know to look for the differences.
What’s Being Done to Fix It?
Health agencies aren’t ignoring this.
The FDA launched its "It’s the Same Medicine" campaign in 2020. It’s simple: clear, plain-language messaging explaining that generics are required to meet the same safety and effectiveness standards. In a pilot across 12 health systems, patient concerns about generics dropped by 28% in six months.
Some pharmacies are now adding a line to generic labels: "Therapeutically equivalent to [Brand Name]." A 2023 trial showed this small change cut discontinuation rates from 52% to 37%.
The Generic Pharmaceutical Association also launched "Generic You Can Count On" in January 2024-a $50 million public education push.
But these efforts are still small compared to the scale of the problem.

Why This Matters for Your Health
If you’re taking a generic drug and you’re feeling unsure-ask yourself: Is it the pill? Or is it the label?
Here’s what you can do:
- Don’t assume a generic is weaker. It’s not. The FDA requires it to be bioequivalent.
- If you notice a change in how you feel after switching, talk to your doctor or pharmacist-not your neighbor or Google.
- Ask if your pharmacy can use a generic labeled with "therapeutically equivalent to [Brand Name]." It makes a difference.
- Don’t stop taking your medication because you think it’s "not working." Give it time. And track your symptoms.
And if you’re a provider? Don’t just say, "It’s the same." Say: "This is the exact same medicine, made to the same standards, just without the marketing. It’s safe. It’s effective. And it’s saving you money."
Is the Labeling Effect Real in Real Life?
Some experts argue that in the real world, cost and convenience matter more than labels. Dr. Aaron Kesselheim from Harvard says the effect might be strong in labs, but in clinics, it’s drowned out by bigger barriers like price, pill burden, and access.
But here’s the problem: if you’re already struggling to take your meds, a tiny drop in confidence can be the last straw. And for chronic conditions, adherence is everything.
The World Health Organization says only about half of people with long-term illnesses take their meds as prescribed. The labeling effect doesn’t cause all of that-but it adds to it.
And with generics making up 90.5% of all prescriptions filled in the U.S., even a small drop in adherence adds up. Experts estimate that if labeling concerns continue unchecked, the U.S. could lose $15 billion a year in savings from avoided hospitalizations, ER visits, and complications.
The Future of Drug Labels
The next step? Smarter labeling.
The Duke-Margolis Center for Health Policy predicts that within five years, drug labels will be risk-proportionate. High-risk drugs-like blood thinners or seizure meds-will have stricter, more detailed labeling that matches the brand exactly. Lower-risk drugs might get simpler, clearer labels.
Some researchers are even testing color-coded labels or QR codes that link to short videos explaining equivalence. The goal isn’t to trick people. It’s to build trust.
Because here’s the truth: generics aren’t second-rate. They’re the backbone of affordable care. But if we keep treating them like second-class medicine, we’ll keep getting second-class results.
It’s not about the pill. It’s about the perception. And perception, in medicine, is power.


Comments (13)
Karandeep Singh
generic is just as good stop being soft
Debbie Naquin
The labeling effect is a manifestation of anticipatory cognition shaping somatic response trajectories. The pharmacological equivalence is ontologically irrelevant when semiotic cues override neurochemical fidelity. The mind doesn't distinguish active ingredients-it distinguishes narratives.
Erin Nemo
I switched to generic lisinopril last year and felt zero difference. My BP is stable. 🙃
elizabeth muzichuk
People are so gullible. They think a label changes chemistry. It’s like blaming the wrapper for the candy inside. This is why America is falling apart. 🤦♀️
Mary Ngo
This is the ultimate control mechanism. Big Pharma doesn’t want you to know that the same molecule can be sold for 90% less. The label is a psychological weapon. They profit from your fear. The FDA? Complicit. The system is rigged.
James Allen
I love how Americans think a pill needs a fancy logo to work. In Russia, we take whatever’s in the box and it works fine. We don’t need marketing to tell us our medicine is real. This is why we’re better at health care.
Scotia Corley
The data is clear. The psychological burden of perceived inferiority reduces adherence. This is not a trivial phenomenon. It is a clinically significant behavioral barrier to therapeutic success. Dismiss it at your peril.
amit kuamr
generic works fine if you dont overthink it people are too emotional about pills
ariel nicholas
Wait-so you’re saying the placebo effect is *stronger* when you’re told it’s branded? That’s not science-that’s manipulation. The entire pharmaceutical industry is built on exploiting cognitive biases. And now they’re weaponizing the word ‘generic’ to keep prices high? This is unethical.
Rachel Stanton
As a pharmacist, I’ve seen this firsthand. Patients will say, 'This generic made me nauseous!'-but it’s the exact same pill they took last month. The only difference? The label changed. We now add 'Therapeutically Equivalent' in bold on the sticker. Adherence jumped 22%. Trust matters more than chemistry sometimes.
Amber-Lynn Quinata
I hate that I’m one of those people who thinks generics don’t work 😭 I feel so dumb but I swear I get worse headaches with them... is it me? Am I broken? 🤕
Charlotte Collins
The real scandal isn’t the labeling effect-it’s that the FDA allows generic manufacturers to omit critical warnings about inactive ingredients. I’ve seen patients have anaphylaxis to dyes or fillers that weren’t listed clearly. This isn’t about perception. It’s about negligence.
Margaret Stearns
I switched to generic metformin after my insurance made me. No side effects. No drop in energy. Just saved $45 a month. Sometimes the simplest truths are the ones we forget.