Thiopurine Dosing Adjustment Calculator
Safe Dosing Calculator
For patients with thiopurine shunting (high 6-MMP levels)
Important: Only use this calculator for patients under specialist care with confirmed thiopurine shunting. Never use for standard azathioprine therapy. Combination requires strict monitoring.
Adjusted Dose Range
WARNING: If you're not a thiopurine shunter, DO NOT combine these medications. Allopurinol with standard azathioprine doses can cause life-threatening bone marrow suppression. Always consult a specialist before adjusting doses.
Combining allopurinol and azathioprine might seem like a simple fix for someone with both gout and an autoimmune condition-but it’s one of the most dangerous drug interactions in modern medicine. This isn’t a theoretical risk. It’s caused real hospitalizations, life-threatening drops in blood cell counts, and even deaths. And yet, many patients and doctors still don’t know about it.
Why This Interaction Is So Dangerous
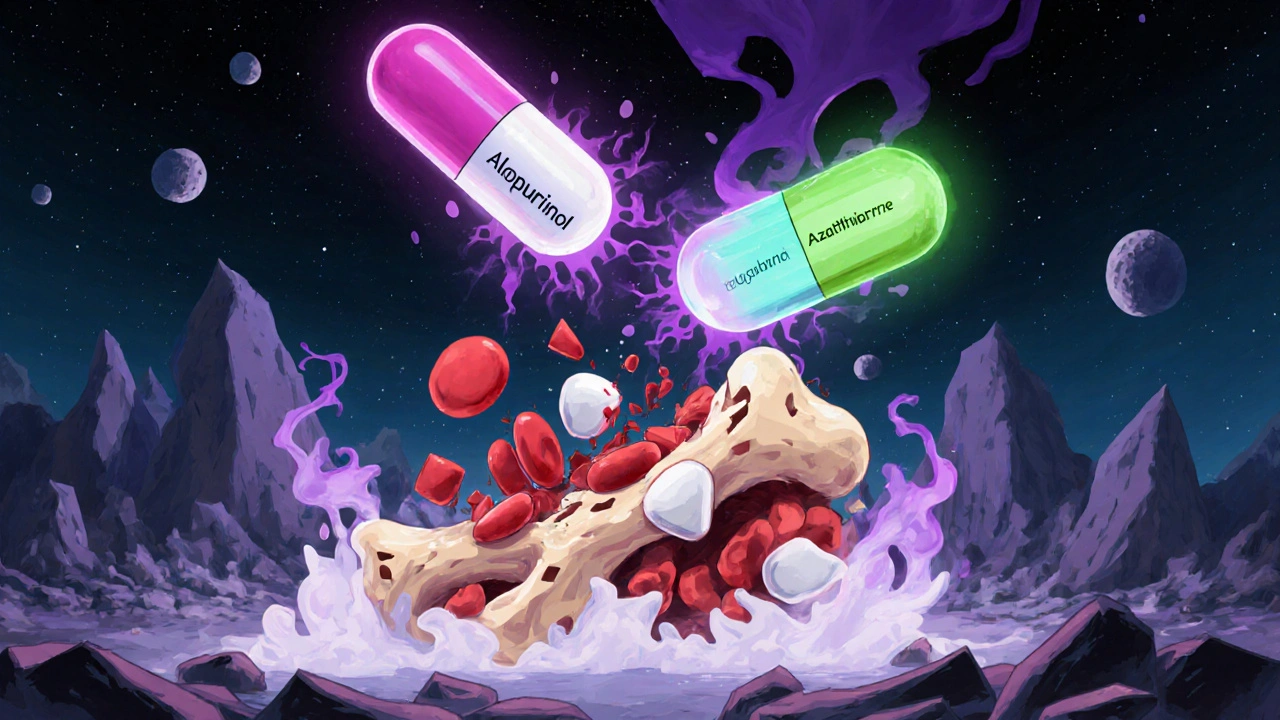
Allopurinol is a common gout medication. It works by blocking xanthine oxidase, an enzyme that makes uric acid. Less uric acid means fewer painful gout flares. Azathioprine, on the other hand, is an immunosuppressant used for Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and after organ transplants. It’s broken down in the body into 6-mercaptopurine (6-MP), which then gets processed by several enzymes to either become active (and therapeutic) or inactive (and harmless). Here’s where the problem starts: allopurinol shuts down one of those key enzymes. When xanthine oxidase is blocked, 6-MP can’t be safely cleared. Instead, it gets redirected into a different pathway that creates too much of the active form-thioguanine nucleotides (6-TGN). This floods the bone marrow, which is responsible for making white blood cells, red blood cells, and platelets. The result? Bone marrow suppression. White blood cell counts can plunge below 1,000/mm³ (normal is 4,000-11,000). Neutrophils-the body’s first line of defense against infection-can drop below 500/mm³. Platelets may fall below 20,000/mm³, leading to uncontrolled bleeding. Hemoglobin can crash to 3.7 g/dL, causing severe anemia. In one documented case from 1996, a patient needed four blood transfusions and intensive care after this interaction occurred.A Real Case That Changed Guidelines
In 1996, a 63-year-old heart transplant patient was prescribed allopurinol for what his doctor thought was gout in his wrist. He was already on azathioprine to prevent organ rejection. Within weeks, his blood counts collapsed. He developed pancytopenia-his body stopped making all types of blood cells. He was hospitalized for weeks. The treatment cost over $13,000 in 1996 dollars (about $25,000 today). He survived, but barely. This case, published by DT Kennedy and colleagues, became a landmark. It was the first time this deadly interaction was clearly documented and linked to a lack of awareness. Since then, the FDA added a black box warning to azathioprine’s labeling-the strongest warning possible. It says: “Concomitant use with allopurinol may cause severe bone marrow suppression.”When Is This Combination Actually Used?
You might be thinking: “If it’s this dangerous, why do doctors ever use it?” There’s one exception: a subset of inflammatory bowel disease (IBD) patients called “thiopurine shunters.” These people metabolize azathioprine into a toxic byproduct called 6-MMP instead of the helpful 6-TGN. High 6-MMP causes liver damage-not bone marrow suppression-but it also means the drug isn’t working to control their IBD. They’re stuck: their disease flares, and their liver gets damaged. For these patients, adding a low dose of allopurinol can redirect metabolism. It shuts down the pathway that makes 6-MMP and pushes the drug toward 6-TGN, the therapeutic form. In a 2018 trial, 53% of these patients achieved steroid-free remission after using allopurinol with a drastically reduced azathioprine dose. But here’s the catch: this only works under strict supervision. The azathioprine dose must be cut to 25-33% of normal (e.g., from 2 mg/kg/day to 0.5-0.7 mg/kg/day). Allopurinol is started at 100 mg/day. Blood tests must be done weekly for the first month, then every two weeks, then monthly. Thiopurine metabolite levels (6-TGN and 6-MMP) must be tracked with specialized lab tests. This isn’t something a primary care doctor can manage. It requires a gastroenterologist or pharmacist with deep expertise in thiopurine metabolism. Only about 32% of U.S. gastroenterologists have ever used this combo, and almost all of them work in academic centers.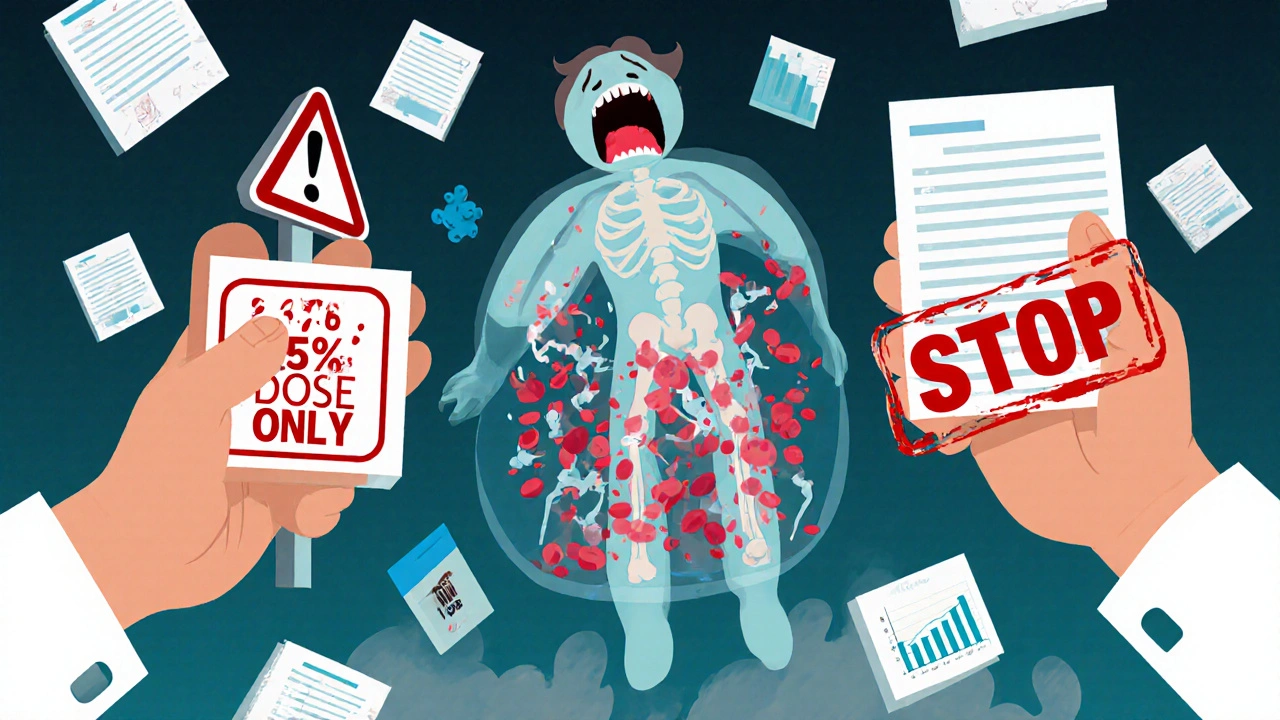
What Happens If You Don’t Adjust the Dose?
If a patient on standard-dose azathioprine (say, 150 mg/day) starts allopurinol without reducing the azathioprine, their 6-MP levels can spike by up to four times. That’s not a small increase. That’s a toxic overload. Symptoms don’t always show up right away. Patients might feel tired, get frequent infections, or notice easy bruising. By the time they go to the ER, their white blood cell count may already be dangerously low. In some cases, the bone marrow damage is so severe that patients need growth factor injections like GM-CSF to kickstart blood cell production. The financial cost is staggering. Hospitalization for severe myelosuppression can exceed $50,000 today. But the human cost is worse: lost time at work, missed family events, fear of infection, and the trauma of nearly dying from a preventable mistake.How to Stay Safe
If you’re on azathioprine and your doctor suggests allopurinol for gout, stop. Don’t start. Ask: “Is there another option?” There are alternatives. For gout, febuxostat is another xanthine oxidase inhibitor-but it doesn’t interact with azathioprine. Pegloticase is an IV treatment for severe gout that bypasses the liver entirely. For IBD, biologics like infliximab or vedolizumab can replace azathioprine without the same risks. If you’re already on both drugs, get your blood tested immediately. Ask your pharmacist or doctor to check your complete blood count (CBC) and thiopurine metabolite levels. If you’ve been on both for more than a few weeks without monitoring, you’re at risk.
Who Should Be Warned?
This isn’t just a doctor’s problem. Patients need to know too. The New Zealand Medicines Safety Authority (Medsafe) explicitly says: “The patient should be warned that azathioprine interacts with allopurinol, a treatment for gout.” If you’re taking azathioprine and your primary care doctor prescribes allopurinol, say: “I’m on azathioprine. Is this safe?” If they say yes without checking your meds list, get a second opinion. Pharmacists are often the last line of defense. Make sure your pharmacy has your full medication list. If you fill a prescription for allopurinol while on azathioprine, the pharmacist should flag it. If they don’t, ask why.The Bigger Picture
About 9.2 million Americans have gout. About 1.6 million have IBD. That’s a lot of potential overlap. Around 25-30% of IBD patients are thiopurine shunters-meaning 400,000 to 480,000 people could theoretically benefit from the combo. But only a tiny fraction do, because the risks are high and the monitoring is intense. The good news? Research is improving. The 2023 TAILOR-IBD trial is testing personalized dosing based on metabolite levels, and early results show remission rates of 68% at one year with careful management. But this isn’t a cure-all. It’s a high-stakes tool for a narrow group of patients. For most people, the safest answer is simple: avoid combining allopurinol and azathioprine. Always. Unless you’re under the direct care of a specialist who’s tracking your blood and metabolites every single week.What to Do Next
- If you’re on azathioprine and need gout treatment, ask your doctor about febuxostat or pegloticase instead of allopurinol.
- If you’re already taking both drugs, get a CBC and thiopurine metabolite test immediately.
- Never start allopurinol without telling your doctor you’re on azathioprine-or 6-mercaptopurine, which has the same risk.
- Ask your pharmacist to review your entire medication list for interactions.
- If you’re an IBD patient and your current treatment isn’t working, ask about thiopurine shunting and whether metabolite testing is right for you.
This interaction isn’t rare. It’s preventable. But only if you know to look for it.

Comments (11)
Emil Tompkins
So let me get this right-you're telling me the entire medical system is just waiting for someone to die before they update a warning label? I've been on azathioprine for 7 years and my PCP just prescribed me allopurinol last month. I'm not even mad, I'm just impressed at how efficiently we're all being slowly poisoned by bureaucracy.
Kevin Stone
I don't know who wrote this but they clearly have no idea how medicine works. Allopurinol is cheap, widely available, and has been used for decades. If you're going to scare people into avoiding it, at least mention that febuxostat costs 10x more and isn't covered by most insurance. This isn't a horror story-it's a cost-benefit analysis.
Natalie Eippert
This is exactly why we need stricter oversight. In the US we let anyone with a medical degree prescribe anything without checking interactions. In New Zealand, pharmacists are legally required to flag this combo. Why can't we do the same here? It's not rocket science-it's basic patient safety.
kendall miles
You know what's really dangerous? The fact that the FDA only added the black box warning after someone almost died. That's not regulation-that's damage control. The real story is that Big Pharma knew about this interaction since the 80s and buried it because they made more money selling azathioprine than alternatives. Wake up people.
Gary Fitsimmons
I have a friend who went through this. He was on both meds for years, never got tested, and ended up in the hospital with a WBC of 300. He's fine now but he says he wishes he'd just asked someone sooner. Don't wait for symptoms. Ask. Now.
Bob Martin
Oh wow. A 2023 trial showing 68% remission rates? And you're telling me to avoid the combo? Bro. That's like saying don't use a chainsaw because it can cut your finger off. Use it right. Or don't use it at all. But don't pretend the tool is the problem.
Sage Druce
This is the kind of post that saves lives. Thank you for taking the time to lay this out so clearly. If you're reading this and you're on azathioprine-don't wait. Talk to your doctor. Talk to your pharmacist. Ask for the metabolite test. You deserve to be safe.
Tyler Mofield
The concomitant administration of allopurinol with azathioprine constitutes a pharmacokinetic interaction mediated by xanthine oxidase inhibition, resulting in elevated 6-TGN concentrations and consequent myelosuppression. This is not a clinical nuance-it is a Class I contraindication per FDA labeling and should be treated as such in all practice settings.
Patrick Dwyer
I work in a GI clinic and we use this combo all the time-but only with metabolite monitoring. It's not about fear. It's about precision. The same way we don't just give chemo without blood counts, we don't give this combo without knowing what's happening inside the body. This isn't risky-it's advanced.
Bart Capoen
I had no idea this was even a thing. I'm on azathioprine for my Crohn's and my doc just put me on allopurinol for gout last month. I just called the pharmacy and they said they didn't flag it because my profile didn't show any 'red flags'. I'm getting my blood drawn tomorrow. Thanks for the heads up.
luna dream
They're hiding this because they want you dependent on drugs. The real cure for gout is alkaline diets and avoiding gluten. The whole medical system is rigged to keep you sick so they can keep selling you pills.