Amoeba Infection Risk Calculator
How Temperature Affects Infection Risk
The article explains that a 0.5°C rise in average water temperature increases reported PAM cases by 12%. This calculator shows how climate change impacts the risk of Naegleria fowleri infection.
Naegleria fowleri thrives in warm freshwater. As temperatures rise due to climate change, its geographic range expands, increasing infection risk for communities near lakes, rivers, and hot springs.
Risk Results
Enter values above to see infection risk calculations.
Note: According to the WHO 2023 climate-health report, a 0.5°C rise in water temperature leads to a 12% increase in reported PAM cases.
When we talk about amoeba infections, we’re dealing with diseases caused by single‑cell protozoan parasites that slip into the human body, usually through contaminated water or food. The notion of wiping them out worldwide sounds simple, but the reality is a tangle of biology, environment, and health‑system hurdles.
Key Takeaways
- Environmental resilience and climate change keep parasite habitats expanding.
- Diagnostic tools are scarce in low‑resource areas, leading to under‑reporting.
- Treatment options are limited and face drug‑resistance concerns.
- Global surveillance is fragmented, hampering coordinated action.
- Investment in water safety, lab capacity, and community education is essential.
Understanding Amoeba Infections
Amoeba infections are diseases caused by free‑living or intestinal protozoa that can invade the gut, liver, brain, or eyes, depending on the species involved. The two most notorious culprits are Entamoeba histolytica the parasite behind amoebic dysentery and liver abscesses and Naegleria fowleri the brain‑eating amoeba that causes primary amoebic meningoencephalitis (PAM). While the former spreads through fecal‑oral routes, the latter thrives in warm freshwater and can enter the nose during swimming.
Major Pathogens and Their Impact
Globally, an estimated 50million people suffer from symptomatic amoebiasis each year, with a death toll of roughly 100,000. In contrast, Naegleria fowleri infects fewer than 150 individuals annually but carries a mortality rate exceeding 95%. These numbers illustrate a paradox: a highly prevalent, often chronic disease versus a rare, almost always fatal infection.
Why Eradication Is Tough
Several interlocking factors keep the global community from declaring victory.
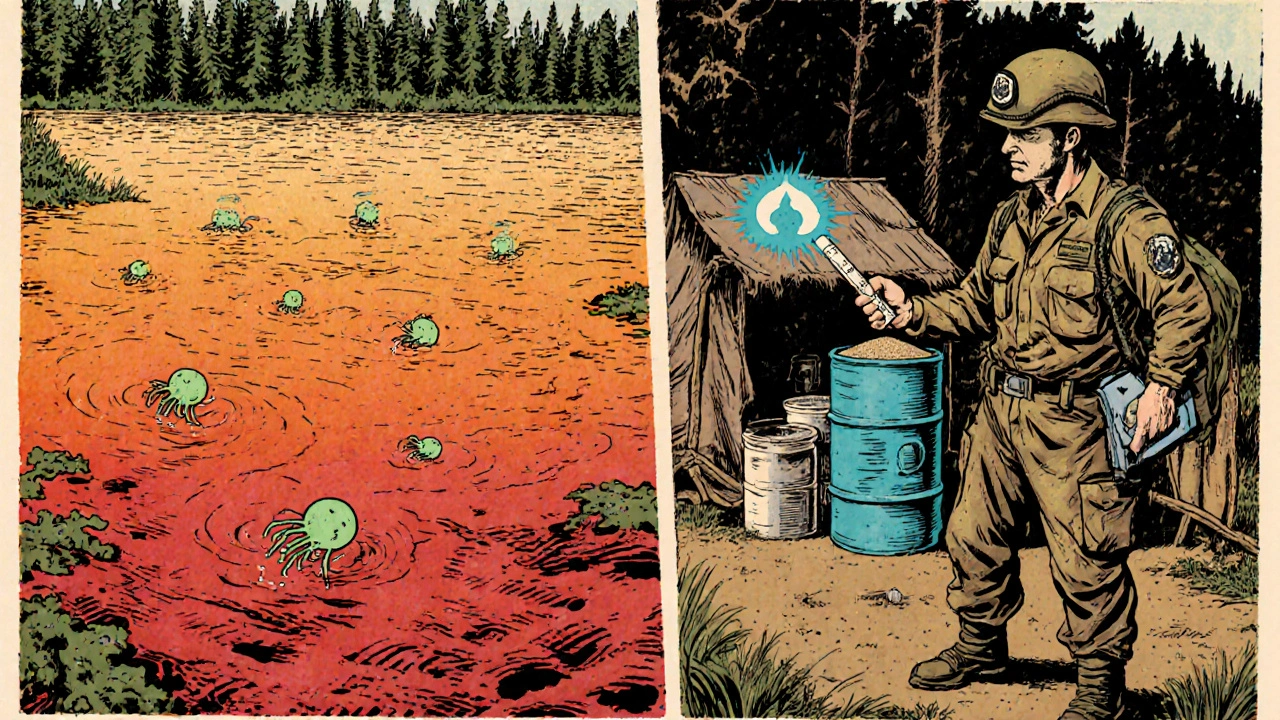
Environmental Resilience
Both Entamoeba histolytica cysts and Naegleria fowleri trophozoites survive in harsh conditions. Climate change is warming lakes and rivers, widening the geographic range where Naegleria fowleri can flourish. A 2023 WHO climate‑health report linked a 0.5°C rise in average water temperature to a 12% increase in reported PAM cases.
Diagnostic Gaps
Rapid, accurate diagnosis requires laboratory infrastructure that many low‑income countries lack. Traditional stool microscopy for Entamoeba histolytica can’t reliably differentiate it from non‑pathogenic cousins like E. dispar. Molecular PCR tests exist but are costly. Consequently, under‑reporting skews surveillance data, making it hard to allocate resources effectively.
Treatment Limitations
The frontline anti‑amoebic drug is metronidazole an antibiotic‑type medication that disrupts DNA synthesis in anaerobic organisms. While effective for intestinal disease, it fails to cross the blood‑brain barrier, leaving PAM patients dependent on experimental regimens like miltefosine, which remains unavailable in many regions. Emerging drug‑resistance signals call for new pharmacological research.
Surveillance Challenges
International bodies such as the World Health Organization (WHO) the United Nations agency coordinating global health responses and the Centers for Disease Control and Prevention (CDC) the U.S. federal public‑health agency that provides technical assistance worldwide maintain databases, but reporting is uneven. Many endemic nations submit data irregularly, and there’s no single, unified platform for amoebic disease metrics.
Socio‑Economic Factors
Poor sanitation, limited access to clean water, and inadequate health education create fertile ground for transmission. In rural South Asia, for example, over 70% of households rely on untreated surface water, a prime source for cysts. Addressing these root causes requires multi‑sector investment beyond the health ministry.
Global Initiatives and Gaps
Efforts to curb amoeba infections fall into three broad categories: policy, research, and implementation.
Policy Frameworks
The WHO’s Water‑Related Diseases Strategy 2022‑2030 sets targets for safe drinking water coverage, yet specific amoeba metrics are missing. The CDC’s Emerging Infections Program includes amoebiasis in its surveillance pilot, but funding caps limit expansion.
Research Investments
Only a handful of clinical trials focus on anti‑amoebic agents, reflecting the low commercial incentive. Non‑profit foundations have funded field studies on rapid diagnostic kits, but scaling remains a hurdle.
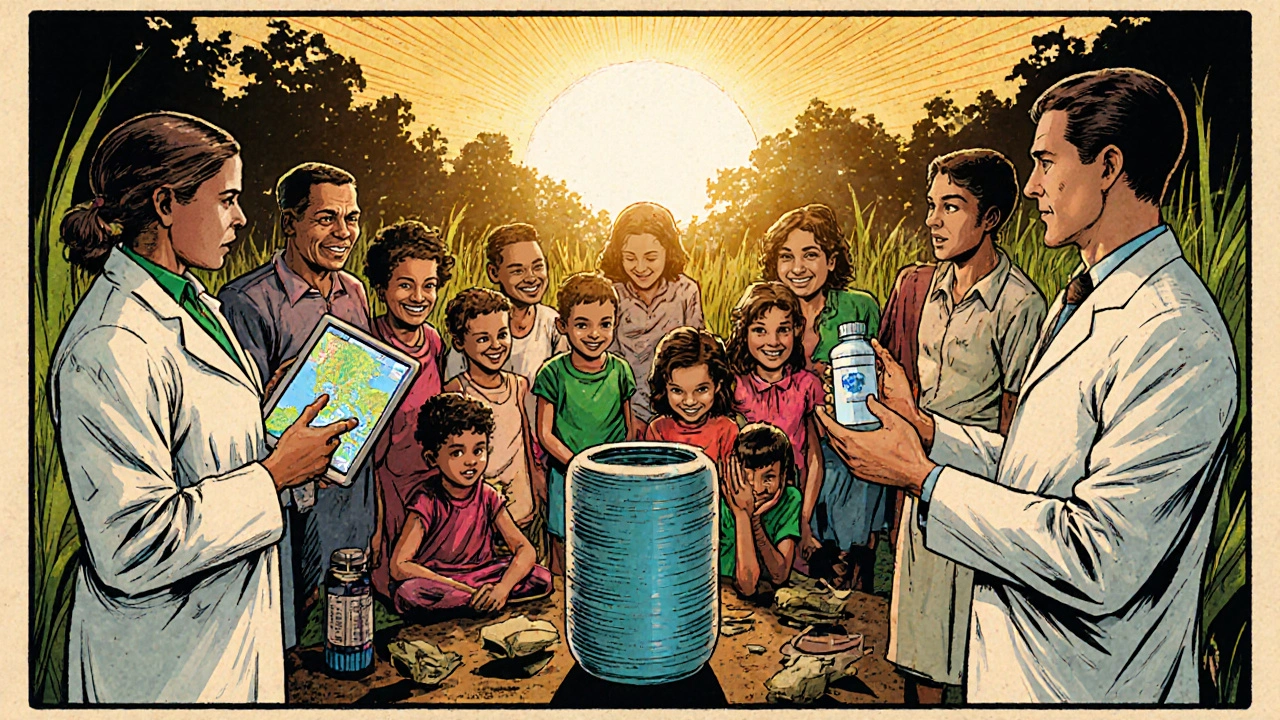
Implementation on the Ground
Community‑based water filtration projects in Kenya have reduced diarrheal disease by 30%, indirectly cutting amoebic cases. However, without routine screening, the true impact is hard to quantify.
Practical Steps Forward
Breaking the stalemate demands coordinated action across several fronts.
Strengthen Water Safety
Deploy low‑cost filtration systems (e.g., ceramic filters) in high‑risk regions. Pair hardware with behavior‑change campaigns that teach families to boil water for at least one minute.
Boost Diagnostic Capacity
Introduce point‑of‑care antigen tests for Entamoeba histolytica that require minimal lab equipment. Train community health workers to collect and preserve stool samples for PCR confirmation at regional labs.
Expand Treatment Options
Prioritize research into oral agents that cross the blood‑brain barrier, such as novel nitroimidazoles. Encourage pharmaceutical partnerships that include “access‑price” clauses for low‑income markets.
Unify Surveillance
Develop an open‑source, cloud‑based reporting platform that integrates WHO, CDC, and national data streams. Use GIS mapping to pinpoint outbreak hotspots and direct resources in real time.
Address Climate‑Related Risks
Incorporate amoeba risk modeling into national climate adaptation plans. Early‑warning systems that track lake temperature spikes can trigger public advisories against swimming.
Challenge vs. Solution Comparison
| Challenge | Mitigation Strategy | Key Stakeholders |
|---|---|---|
| Environmental resilience and climate‑driven range expansion | Integrate temperature‑based risk maps into public health alerts | Environmental agencies, WHO, local governments |
| Limited diagnostic infrastructure | Deploy point‑of‑care antigen kits; train community health workers | Ministries of Health, NGOs, diagnostic manufacturers |
| Scarce effective therapies for brain infections | Fund research on blood‑brain‑penetrant drugs; negotiate access pricing | Pharma companies, research institutions, global funders |
| Fragmented surveillance data | Adopt a unified, cloud‑based reporting platform with GIS capabilities | WHO, CDC, national disease control centers |
| Poor water and sanitation | Scale low‑cost filtration, promote boiling, improve sewage treatment | Development banks, NGOs, local water authorities |
Frequently Asked Questions
What are the most common symptoms of amoebiasis?
Typical signs include abdominal pain, diarrhea with blood or mucus, and fever. In severe cases, the parasite can invade the liver, causing a painful abscess.
How is Naegleria fowleri transmitted?
The organism lives in warm freshwater. Infection occurs when contaminated water forces its way up the nose, usually during activities like swimming, diving, or water‑sports.
Can drinking water filters remove amoeba cysts?
Yes, filters rated at 0.2µm or smaller can trap cysts of Entamoeba histolytica. However, regular maintenance is crucial to keep performance high.
Why is there no vaccine for amoeba infections?
Developing a vaccine is challenging because the parasites can change surface proteins to evade immunity. Funding and limited commercial interest have also slowed progress.
What role does climate change play in the spread of amoebic diseases?
Warmer temperatures increase water bodies’ suitability for thermophilic amoebae like Naegleria fowleri. This expands its geographic range and raises the risk of exposure for communities that previously were safe.
Next Steps for Stakeholders
Governments should embed amoeba‑specific targets into national water‑safety plans, while donors must earmark funds for diagnostic kit rollout. Researchers need collaborative platforms to share data on drug efficacy, and community leaders should champion simple hygiene habits like regular hand‑washing and water‑boiling.
Eradicating amoeba infections won’t happen overnight, but coordinated, evidence‑based actions can dramatically cut disease burden and move us closer to a world where these hidden parasites no longer threaten public health.

Comments (11)
Ari Kusumo Wibowo
Look, we can’t keep throwing band‑aid solutions at a problem that needs a global playbook – we need coordinated water safety standards, shared diagnostic tech, and a no‑excuses stance on funding, otherwise the same parasites keep coming back.
Hannah Gorman
While the enthusiasm for quick fixes is understandable, we must acknowledge that the epidemiological data underpinning amoebic disease control is riddled with methodological flaws, and the casual reader often overlooks the nuanced interplay between climate change and pathogen ecology. The first misstep is assuming that a single‑point intervention, such as distributing ceramic filters, will linearly translate into reduced incidence without accounting for cultural adherence to boiling practices. Second, the reliance on PCR in low‑resource settings is unrealistic unless we address the supply chain constraints that make reagents prohibitively expensive. Third, the narrative that drug resistance is merely a future concern fails to recognize the documented cases of metronidazole tolerance in Southeast Asian cohorts. Fourth, surveillance fragmentation is not a mere bureaucratic inconvenience; it leads to under‑reporting that skews global burden estimates, thus depriving high‑risk regions of necessary aid. Fifth, the health‑education campaigns cited often lack longitudinal assessment, rendering their impact anecdotal at best. Sixth, the climate‑driven expansion of Naegleria fowleri habitats is not a hypothetical scenario but a documented phenomenon in previously temperate zones, demanding preemptive public health advisories. Seventh, the ethical implications of “access‑price” clauses in pharmaceutical agreements must be scrutinized to prevent inadvertent exploitation. Eighth, community‑based interventions must be integrated with national policy frameworks to ensure sustainability beyond grant cycles. Ninth, the role of local NGOs in bridging the gap between laboratory capacity and field deployment is undervalued in most strategic plans. Tenth, the notion that “more funding” is a panacea ignores the necessity of targeted, outcome‑driven allocation. Eleventh, the potential for multiplex rapid diagnostic kits remains untapped due to regulatory inertia. Twelfth, the psychological burden on patients in endemic areas is rarely addressed, despite its impact on treatment adherence. Thirteenth, interdisciplinary collaborations between climatologists, epidemiologists, and engineers are essential yet seldom operationalized. Fourteenth, the sociopolitical dimensions of water governance, especially in transboundary river systems, add a layer of complexity that cannot be circumvented. Fifteenth, without an open‑source data platform, researchers are forced to work in silos, perpetuating duplication of effort. In sum, the eradication of amoeba infections is not a simple checklist but a multidimensional challenge that demands strategic foresight, rigorous evaluation, and unwavering commitment.
Tatiana Akimova
Alright team, let’s crank up the energy – we have the tools, we have the data, and we have the urgency, so why are we still stuck at the discussion stage? Deploy point‑of‑care antigen kits now, train every community health worker on sample handling, and push for a “boil‑water‑for‑60‑seconds” campaign that actually gets on radio and TikTok. The clock is ticking and every day we wait costs lives, especially where the brain‑eating Naegleria is creeping north.
Calandra Harris
We must recognize that the Western‑centric model of health intervention ignores the sovereign right of nations to manage their own water resources Its a philosophical error to impose one‑size‑fits‑all solutions without respecting local autonomy The true solution lies in harmonizing global science with national pride and indigenous knowledge
Dan Burbank
Witness, dear colleagues, the tragedy of a world that lets a microscopic tyrant dictate the fate of nations! The drama unfolds as climate‑warriors watch lakes warm, while policymakers clutch flimsy spreadsheets. Yet, behold – the dramatic crescendo: a single, elegant filter, a meticulously engineered PCR assay, a bold treaty signed under the aurora of hope. Does it not stir the soul to imagine laboratories humming in remote villages, each test a stanza in the epic of eradication? Let us not merely whisper in conference halls; let us roar in the streets, for the stakes are nothing less than the reclamation of human dignity from a hidden foe!
Anna Marie
Dear colleagues, I appreciate the depth of discussion and would like to add a note of collaboration. It is essential that we align our strategic objectives with the capacities of local health ministries and ensure that any diagnostic rollout is accompanied by thorough training modules. Moreover, the formal adoption of water‑safety protocols must be coupled with community outreach programs that respect cultural practices while promoting evidence‑based measures.
Abdulraheem yahya
From my perspective, the global community has a unique opportunity to leverage existing infrastructure, such as solar‑powered water purification units, to address both the immediate need for safe drinking water and the longer‑term goal of reducing amoebic transmission. By integrating point‑of‑care diagnostics into the routine activities of community health workers, we can create a feedback loop that informs real‑time surveillance and resource allocation. This approach not only maximizes the impact of limited funding but also empowers local stakeholders, fostering sustainability and resilience against future climate‑driven challenges.
Preeti Sharma
It is tempting to accept the dominant narrative that frames amoeba eradication as a linear problem solved by technology alone, yet such a view neglects the dialectic between human agency and environmental contingencies. By questioning the inevitability of the current trajectory, we open space for alternative epistemologies that prioritize adaptive governance over rigid interventionist paradigms.
Ted G
Anyone else notice how the so‑called “global surveillance” networks are actually just a cover for data mining by entities that have ulterior motives? The real agenda seems to be about control, not health.
Miriam Bresticker
Wow!! This post is sooo informative 😃 but I think we need more lemmas about the futere of iiiiiphotical treatments 😂😂
Claire Willett
Deploy GIS-driven alert systems to pre‑empt exposure.